A new Northwestern Medicine study published in Nature Medicine has shown that reprogrammed stem cells can be used to identify patients with cancer who are likely to experience a dangerous side effect of a common chemotherapy drug.
Doxorubicin, also known Adriamycin, effectively treats a wide range of cancers, including breast cancer and pediatric leukemia. But for about 8 percent of patients, the drug causes cardiotoxicity – heart muscle damage so severe that it can lead to heart failure. Currently, healthcare providers can’t predict in advance who will fall into this subset of patients.
“We were interested in whether there is a genetic reason for why some patients experience cardiotoxicity and some do not,” said corresponding author Paul Burridge, PhD, assistant professor of Pharmacology and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
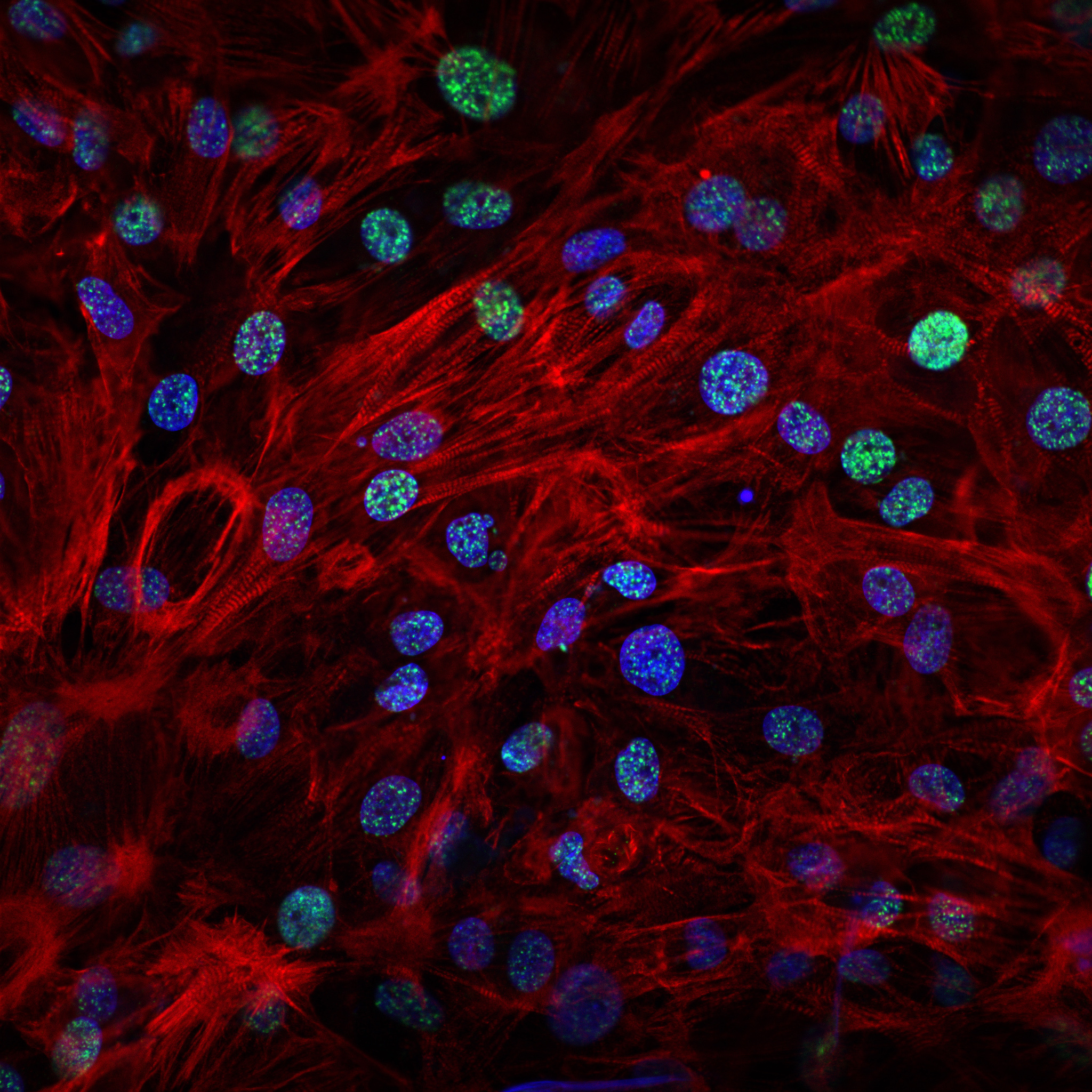
It’s difficult to isolate and grow a patient’s heart cells in a lab, so Burridge took an alternative route to test the drug: stem cells. First, Burridge and scientists at Stanford University acquired skin cells from patients with breast cancer who were treated with doxorubicin – some with cardiotoxicity and some without it. The investigators reprogrammed the skin cells into pluripotent stem cells, which can become many different types of cells.

“We then turned these stem cells into heart muscle cells, treated them with doxorubicin and measured their responses,” Burridge explained. “Our results showed that heart cells from patients who have cardiotoxicity were significantly more sensitive to doxorubicin-induced toxicity. They had more structural damage, reduced contraction, DNA damage and died more easily.”
By analyzing gene expression in the cells, the scientists were able to establish genetic differences in drug response. Their work also suggests that mitochondrial dysfunction could be behind the toxic side effect.
The study’s findings also have implications for clinical care.
“This project proves for the first time that we might be able to predict the likelihood of a patient experiencing doxorubicin-induced cardiotoxicity by looking at the patient’s DNA,” Burridge said. “This patient could then be given an alternative chemotherapy drug or a lower dose. In contrast, patients who are likely to be resistant to doxorubicin-induced cardiotoxicity might be able to be given a higher dose and have a better chance of success with their chemotherapy.”
This study was supported by National Institutes of Health grants K99/R00 HL121177, R21 HL123655, R01 LM05652, R01 GM102365, R24 GM61374, R01 HL123968, R01 HL126527, R01 HL128170, R01 HL130020, R01 AR063963, R01 AG020961, R21 AG04481501, R01 NS089533; American Heart Association grants 14BGIA20480329, 13POST14480004 and 13EIA14420025; a Dixon Translational Research Grant Young Investigator Award; Muscular Dystrophy Association grant 4320; California Institute of Regenerative Medicine grants IT1-06596, TR3-05501 and RB5-07469; Muscular Dystrophy Association grant 4320; the Baxter Foundation; and a Burroughs Wellcome Fund Innovation in Regulatory Science Award.






