Newborns are more susceptible to severe disease from herpes simplex virus (HSV) infection than adults, often leading to encephalitis or swelling of the brain.
By comparing the disease in adults and newborns, Northwestern Medicine scientists have revealed age-related differences in the development of encephalitis and the role of autophagy, the cellular mechanism for degradation of unnecessary cellular components, in the newborn brain.
“We were interested in identifying reasons newborns are so susceptible to herpes, and I’ve always thought the common idea that it’s because newborns lack a mature immune response unsatisfying,” said William J. Muller, MD, PhD, assistant professor of Pediatrics in the Division of Infectious Disease and principal investigator of the study. “So we wanted to find more specific factors for why newborns are more susceptible to encephalitis in this disease and what is different in the central nervous system of adults and newborns.”
In a recently published paper in PLoS Pathogens, Dr. Muller and his team used mouse models to study HSV: they found a viral protein that promotes encephalitis in adults by blocking host autophagy wasn’t required to cause HSV disease in newborns. Instead, the activation of autophagy during the inflammatory response in adults uses a specific signaling pathway; the scientists found in newborn HSV infection, autophagy activation happened via a different signaling pathway.
They also observed an association between the activation of autophagy and increased cell death in newborns but not in the adult brain, which may contribute to the increased amount of disease in newborns.
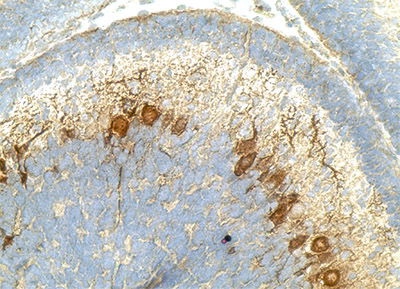
In addition to the mouse models, the scientists showed through human tissue samples the activation of autophagy and cell death in a case of newborn HSV encephalitis.
These differences in the protective role of autophagy in adults have clinical importance, where the development of autophagy-inducing drugs could be beneficial to adults, but detrimental to newborns.
“From a clinical standpoint, we’ve suggested that inducing autophagy is not protective in the newborn,” Dr. Muller said. “There might be differences in the activity of certain agents between adults and newborns and this comes into play when implementing treatments.”
Muller and his team plan to further investigate the gene that activates the autophagy in newborns and find a treatment that may interfere with this gene or its associated signaling pathway.
The lead author of the study is Douglas R. Wilcox, a student in the Medical Scientist Training Program and co-authors include Nitin R. Wadhwani, MD, instructor of Pathology, and Richard Longnecker, PhD, professor of Microbiology-Immunology.
The research was funded by National Institutes of Health grants NCI CA060553, T32AI060523, R01CA021776 and K08AI89942.






