This article was originally published in the Breakthroughs Newsletter. Find more stories like this, as well as the Breakthroughs Podcast, on the Breakthroughs homepage
Parkinson’s disease is a complex illness. Even with an abundance of basic science discoveries, a curative treatment is still out of reach. However, recent advances have powered a new, deeper understanding of the disease that could reveal the last pieces of this decades-long puzzle and pave the way to a disease-modifying treatment.
Outlining the Stages of Disease

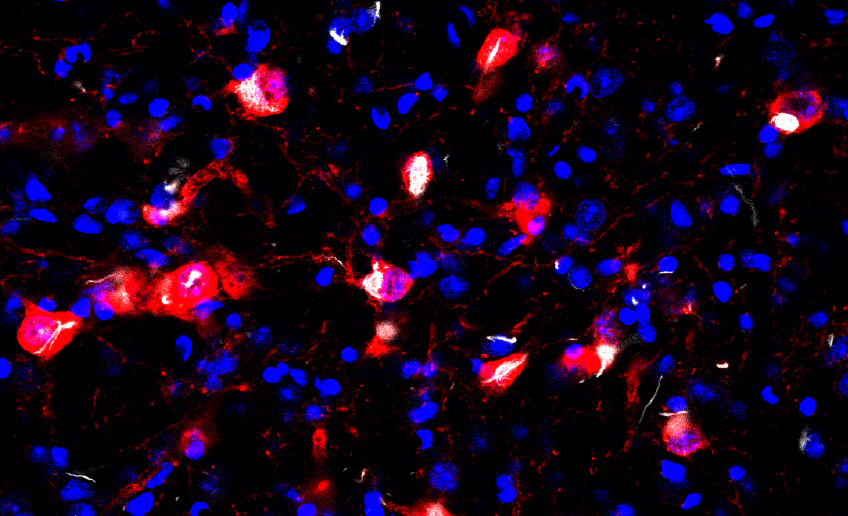
The death of dopamine-producing neurons that innervate the basal ganglia is responsible for the core motor symptoms of Parkinson’s disease (PD), which include slowness of movement and rigidity. In a study published in Nature, D. James Surmeier, PhD, chair and the Nathan Smith Davis Professor of Neuroscience, found that damage to mitochondria — cellular power plants — in mouse dopaminergic neurons produced a progressive “Parkinsonism” closely resembling that seen in humans with PD.
Investigators found that damage to mitochondria first affected the axons of dopaminergic neurons, causing an inability to communicate with distant parts of the brain, particularly a region called the striatum. It had previously been thought that this communication failure was responsible for the movement difficulty experienced by patients with PD. However, Surmeier’s group found that this failure was not enough and resulted in only modest deficits in learning and fine movements. The key impairment in movement only appeared later, when dopaminergic neurons stopped communicating with their closest neighbors in the substantia nigra.
“This suggests that there are at least two major stages in the disease: an early stage where the striatum stops doing its job but where other parts of the brain compensate and a late stage when the basal ganglia begins to disrupt the function of the rest of the brain — this is when symptoms become debilitating,” Surmeier said.
Listen to the Breakthroughs Podcast on this research:
The study also demonstrated the feasibility of a new therapy for patients with late-stage PD that uses a gene therapy to boosting effectiveness of current therapies, whose efficacy wanes as the disease progresses.
“Our study demonstrates that if you can keep dopamine levels up in the substantia nigra, it may be enough keep many of the motor symptoms at bay,” Surmeier said.
Understanding Cell Waste Management
Another major feature of PD is the neuronal protein alpha-synuclein. In healthy cells, the protein helps vesicles travel from neuron to neuron, but in neurons affected by Parkinson’s disease the protein is misfolded, aggregating in large clumps. These clumps in the brain are linked to a variety of harmful effects including oxidative stress, inflammation and mitochondrial dysfunction.

“Why alpha-synuclein aggregates and why can’t the neurons eliminate it, those are the big questions we need to answer,” said Joseph Mazzulli, PhD, associate professor in the Ken and Ruth Davee Department of Neurology in the Division of Movement Disorders.
Mazzulli studies how the lysosome, the organelle responsible for waste disposal in the cell, is impeded by alpha-synuclein. In a recent paper published in Neuron, Mazzulli found that alpha-synuclein-induced lysosomal dysfunction leads to a buildup of malformed proteins that are unable to exit the endoplasmic reticulum and proceed to the lysosome, as would occur in healthy cells. This begets a vicious cycle, where additional proteins aggregate and further impede disposal.
Using patient-derived midbrain neurons modeling the disease, Mazzulli and his collaborators found that an FDA-approved drug — diltiazem — can restore proper folding and prevent clumping of enzymes, representing a possible therapeutic pathway.
“Combining diltiazem with protein trafficking enhancers known as farnesyltransferase inhibitors has shown to be the best strategy for reducing protein aggregates in patient cultures, since they synergistically target two key dysfunctional pathways in PD,” Mazzulli said.
Dimitri Krainc, MD, PhD, the Aaron Montgomery Ward Professor and chairman of the Ken and Ruth Davee Department of Neurology, studies lysosomal and mitochondrial function in PD. According to findings published in Science, dysfunction of these organelles leads to an accumulation of toxic oxidized dopamine that contributes to preferential degeneration of dopaminergic neurons in PD.
A study from the Krainc laboratory published in Nature showed that mitochondria and lysosomes form direct contacts, and recent work published in Nature Communications showed that these contacts are disrupted in PD. Based on these findings, the Krainc laboratory used patient-derived neurons to develop and test a new strategy to treat Parkinson’s disease by mitigating the effects of dysfunctional lysosomes and mitochondria, as detailed in a study published in Science Translational Medicine.
“These key pathological features of PD were only seen in human neurons and not in mouse models, further emphasizing the value of patient-derived neurons for drug development in Parkinson’s disease,” said Krainc, who is also director of the Simpson Querrey Center for Neurogenetics.
Searching for Biomarkers
As the basic mechanisms underlying PD pathogenesis are progressively uncovered, those discoveries are whisked into a therapeutic pipeline of which Feinberg is an important part. Tanya Simuni, MD, the Arthur C. Nielsen, Jr., Research Professor of Parkinson’s Disease and Movement Disorders and director of the Parkinson’s Disease and Movement Disorders Center, is the principal investigator on several ongoing clinical trials, including some testing novel therapeutics. However, the trial that could produce the largest benefit is one that’s not testing drugs at all.
“While a number of diseases routinely use biomarkers in research and clinical practice, Parkinson’s disease still does not have such objective measures,” said Simuni, who is also chief of Movement Disorders in The Ken and Ruth Davee Department of Neurology.
This is one reason why Northwestern is one of 50 institutions participating in the Parkinson’s Progression Markers Initiative (PPMI), a longitudinal clinical and biomarker dataset involving more than 1,400 participants with idiopathic Parkinson’s, individuals with genetic forms of Parkinson’s, participants with early symptoms of the disease, as well as healthy controls. Simuni serves on the study steering committee and has published extensively using PPMI data, including a recent publication in Lancet Neurology detailing ‘soft’ symptoms that appear before the disease affects daily life.
“PPMI data are essential to developing better tools to advance and accelerate novel therapies for this increasingly common disease of aging,” Simuni said.

However, the question of pathways remains: with the variety of pathogenic mechanisms that have been uncovered, devising a single treatment that works for all patients would be exceedingly difficult. Instead, subtyping PD based on genetic mutations and devising specific therapies is the most promising route to a cure, according to Simuni.
“We need to identify the biological signature of individuals’ disease and use that to target the relevant pathways,” Simuni said.
Better biomarkers — genetic or otherwise — would also aid in the ultimate effort: prevention. PD is often progressing silently for years before a patient comes into the clinic with symptoms, Simuni said, so developing methods to identify PD early is critical to preventing the illness.
“We need to intervene before someone develops the full clinical picture of disease,” Simuni said. “To do that, we need biologically-based measures of disease — and that’s what we hope to find with PPMI.”






