Changes to two previously unstudied genes are the centerpiece of a new theory regarding the cause and development of endometriosis, a chronic and painful disease affecting 1 in 10 women.
The discovery by Northwestern Medicine scientists suggests epigenetic modification, a process that enhances or disrupts how DNA is read, is an integral component of the disease and its progression. Matthew Dyson, PhD, research assistant professor of Obstetrics and Gynecology-Reproductive Biology Research and Serdar Bulun, MD, chair of Obstetrics and Gynecology also identified a novel role for a family of key gene regulators in the uterus.
“Until now, the scientific community was looking for a genetic mutation to explain endometriosis,” said Dr. Bulun, a member of the Center for Genetic Medicine and the Robert H. Lurie Comprehensive Cancer Center. “This is the first conclusive demonstration that the disease develops as a result of alterations in the epigenetic landscape and not from classical genetic mutations.”
The findings were published March 6 in PLoS Genetics.
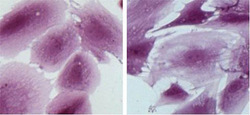
Women develop endometriosis when cells from the lining of the uterus, usually shed during menstruation, grow in other areas of the body. The persistent survival of these cells results in chronic pelvic pain and infertility. Although the cause of the disease has remained unknown on a cellular level, there have been several different models established to explain its development.
Endometriosis only occurs in menstruating primates, suggesting that the unique evolution behind uterine development and menstruation are linked to the disease. Scientists consider retrograde menstruation – cells moving up the fallopian tubes and into the pelvis – as one probable cause.
Previous models, however, have been unable to explain why only 10 percent of women develop the disease when most experience retrograde menstruation at some point. Nor do they explain instances of endometriosis that arise independent of menstruation.
Bulun and Dyson propose that an epigenetic switch permits the expression of the transcription factor GATA6 rather than GATA2, resulting in progesterone resistance and disease development.
“We believe an overwhelming number of these altered cells reach the lining of the abdominal cavity, survive and grow,” said Dr. Bulun, obstetrician-gynecologist-in-chief at Northwestern Memorial’s Prentice Women’s Hospital. “These findings could someday lead to the first noninvasive test for endometriosis.”
Clinicians could then prevent the disease by placing teenagers predisposed to this epigenetic change on a birth control pill regimen, preventing the possibility of retrograde menstruation in the first place.
Dyson will also look to use the epigenetic fingerprint resulting from the presence of GATA6 rather than GATA2 as a potential diagnostic tool, since these epigenetic differences are readily detectable.
“These findings have the potential to shift how we view and treat the disease moving forward,” Dr. Bulun said.
The project was supported by a National Institutes of Health MERIT Award to Dr. Bulun (R37-HD38691) and a grant from the Friends of Prentice.






