Painful Diabetic Neuropathy (PDN), a disorder that causes severe nerve damage throughout the body, affects more than a quarter of diabetes patients.
Daniela Menichella, MD, PhD, assistant professor in Neurology, has established that a specific signaling pathway may lead to the excitability of sensory neurons and inflammation in PDN. The sustained excitability of these neurons reduces the pain threshold of those with the disease.
“We do not fully understand the molecular mechanisms that underlie neuropathic pain in diabetes and we are trying to learn why the sensory neurons that signal pain are expressing higher excitability,” Dr. Menichella said. “In patients with PDN, the pain threshold is lower than in healthy individuals and current therapies are only partially effective.”
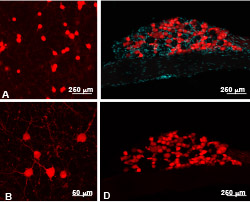
Sensory neurons display excitability in response to different molecules, including chemokines, or signaling proteins. Combining pain behavioral tests, electrophysiology studies, in vitro and in vivo calcium imaging studies, and transgenic mouse models, Dr. Menichella identified chemokine SDF-1 and its receptor CXCR4 as pivotal in the development of PDN.
Part of these research findings have been recently published in Molecular Pain.

“These findings open up a completely new field of molecular investigation in this disease,” she said. “Now that we have identified a possible signaling pathway for the disease, we can create a targeted therapy. By modifying the neurobiology and controlling inflammation, we can not only treat the pain but also slow the progression of the disease.”
Through her investigations, Dr. Menichella also observed that expression of the receptor CXCR4 caused inflammatory cells to go into the sensory neurons.
She now investigates the communication between this excitability in sensory neurons and inflammation.
“As a neurologist, I see patients with PDN and it has a very high impact on the quality of life of the patient. Finding the molecular mechanism, we can develop a targeted therapy and then translate it to patients,” said Dr. Menichella. “Neuropathic pain is found in rheumatologic conditions and hereditary, amyloid and chemotherapy-induced neuropathies. So knowing how inflammation and chemokines control excitability in sensory neurons is a concept that can be applied to other diseases.”
The study is funded by National Institute of Neurological Disorders and Stroke grant K08NS079482.






