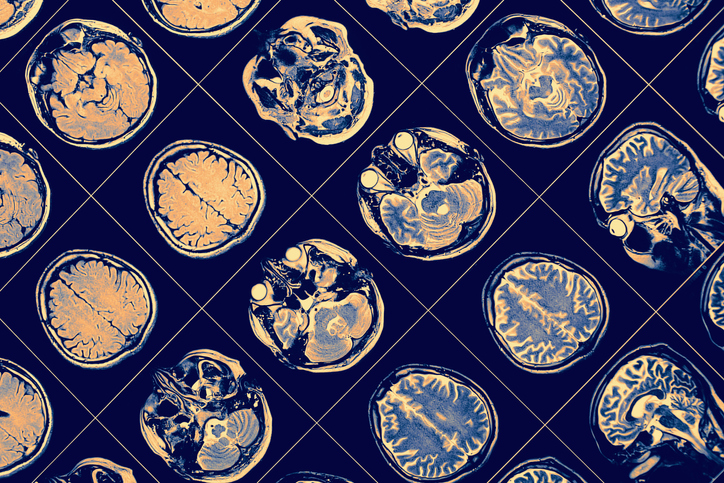
Northwestern Medicine investigators have shown that inhibiting a mutated gene can reduce seizure activity in adult-type diffuse gliomas, according to a study published in the Journal of Clinical Investigation.
Adult‐type diffuse gliomas are the most common malignant tumors arising in the central nervous system, affecting six in 100,000 worldwide, according to the National Institutes of Health.
Most adult-type diffuse glioma patients will experience at least one seizure during the course of the disease and they’re often difficult to control with medication.
Craig M Horbinski, MD, PhD, director of Neuropathology in the Department of Pathology and senior author of the paper, said the idea for the study came to him as he was conducting chart reviews for his glioma patients.

“When during chart reviews for an unrelated study, I discovered that IDH mutant glioma patients seemed to be having a lot of problems with seizures, more so than IDH wild-type glioblastoma patients did,” said Horbinski, who is also director of the Pathology Core Facility at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “That was a little surprising because IDH wildtype glioblastomas are inherently much more aggressive, more tissue destructive. You would think they would cause more seizures in patients, but it was just the opposite. So, we explored it further and found out, yes, there was indeed a patient-based connection where IDH mutant gliomas had more seizures, both before and after surgery.”
Horbinski’s previous research has shown that gliomas with mutations in the IDH (IDHMut) gene are more likely to cause seizures because the mutated gene produces D-2-hydroxyglutarate (D2HG), a chemical which excites neurons and leads to an increase in seizure activity.
In the current study, scientists added either IDHmut or IDH wild-type (IDHwt) cells from glioma patients to human pluripotent stem cell-derived cortical spheroids made up of cortical neurons and glial cells. While spheroids with IDHwt glioma cells showed stable activity, those with IDHmut glioma cells exhibited gradually increasing firing rates.
Investigators then observed that mice grafted with IDHmut glioma cells experienced seizure activity nearly five times as often as mice with IDHwt gliomas.
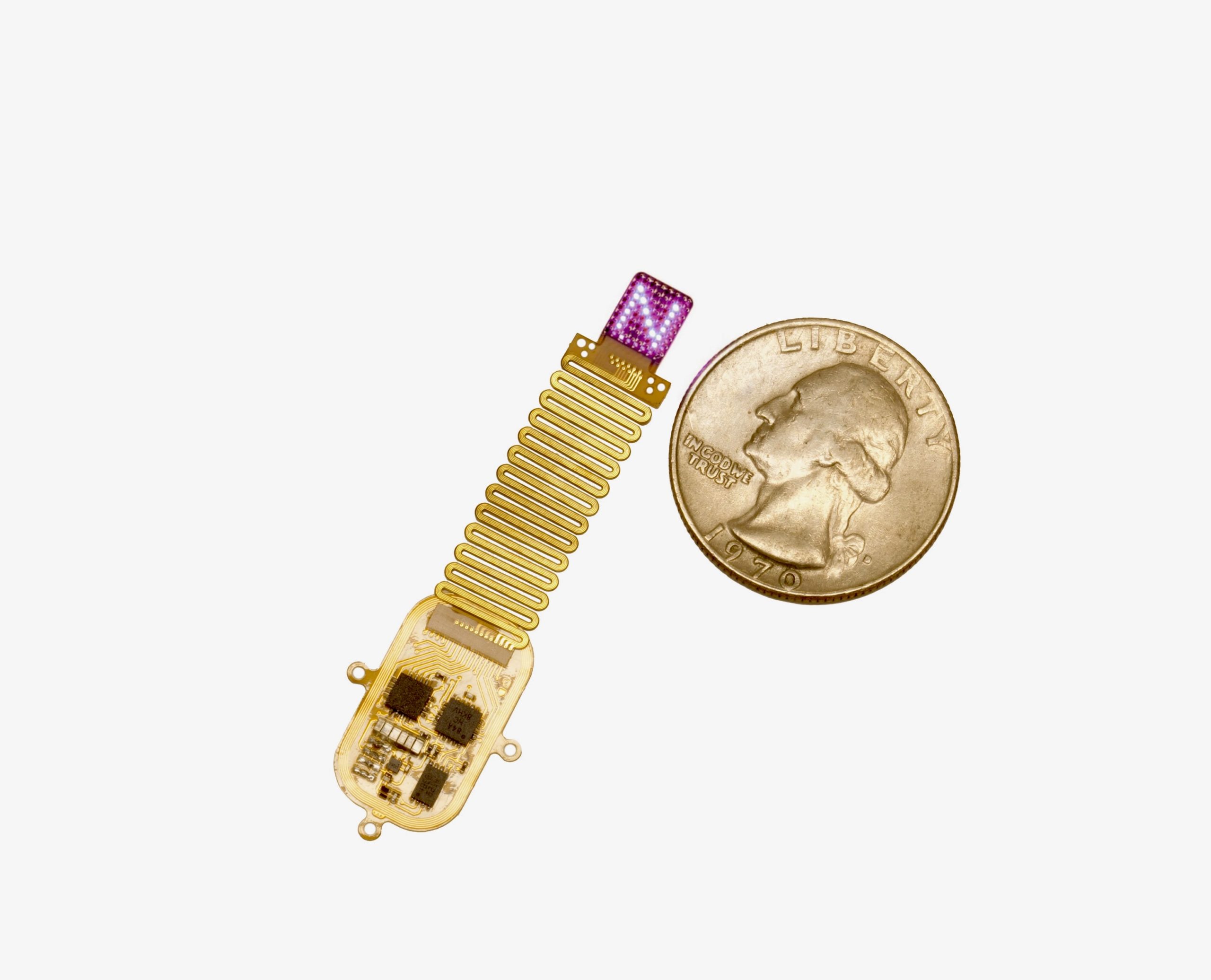
In an effort to inhibit IDHmut, Horbinski and his collaborators introduced AG881, a newly discovered small molecule inhibitor which can cross the blood-brain barrier. The inhibitor reduced seizure activity in mice with IDHmut gliomas by more than 50 percent, according to the study.
“We’ve showed definitively that the chemical product of the IDH mutant enzyme, which is called D-2-hydroxyglutarate, is responsible for causing increased neuronal network bursting, and that’s basically the experimental equivalent of a seizure,” Horbinski said. “We were able to show this in cultured neurons as well as in animal models of IDH mutant gliomas. But what was especially exciting is that we were able to substantially reduce those seizures by treating the cultures as well as the animals with an inhibitor that’s specifically designed to block the IDH mutant enzyme from working.”
The findings provide a basis for treating seizures in human glioma patients, Horbinski said, adding that he and his team will be following multiple international clinical trials already underway to further confirm the results.
“One of the more gratifying aspects of this research is this bedside-to-bench aspect of it,” Horbinski said. “We make patient-based observations for which we really didn’t have any a priori hypotheses, bring them into the laboratory, study them in more detail, and then ultimately bring it out to improve patient care again. So, it’s a bedside-to-bench and then back again. That’s a great dynamic that really helps.”
This work was supported by the Lou and Jean Malnati Brain Tumor Institute of the Lurie Cancer Center, a Specialized Program of Research Excellence (SPORE) in Brain Cancer grant, as well as National Institutes of Health grants R01NS102669, R01NS117104 and R01NS118039.