Inflammation in the heart can mount immune responses even in the absence of immune cells, according to a Northwestern Medicine study published in the Journal of Clinical Investigation.
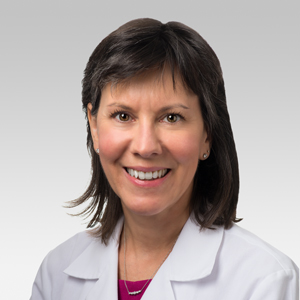
The discovery provides clearer targets for treating myocarditis, or inflammation of the heart muscle, a condition which can develop suddenly after a viral infection, vaccination or due to gene mutations, said Elizabeth McNally, MD, PhD, the Elizabeth J. Ward Professor of Genetic Medicine and director of the Center for Genetic Medicine, who was senior author of the study.
“Myocarditis is when a patient shows up in the emergency room having chest pain, having irregular heart rhythms, and having an inflammation process in their heart that can sometimes cause the heart function to be reduced, and so they can have signs of heart failure,” McNally said. “It can be very serious, and we don’t have a lot of great treatments for it.”
It’s now understood that myocarditis is often linked to mutations in DSP, a gene that encodes for proteins essential for the proper contraction of heart muscles, McNally said.
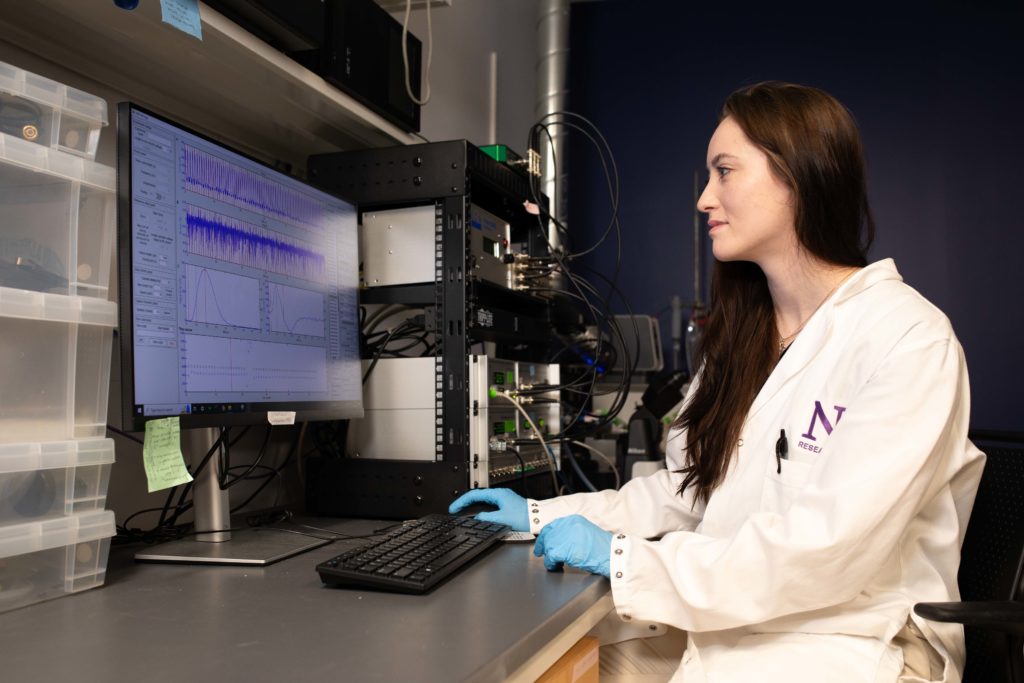
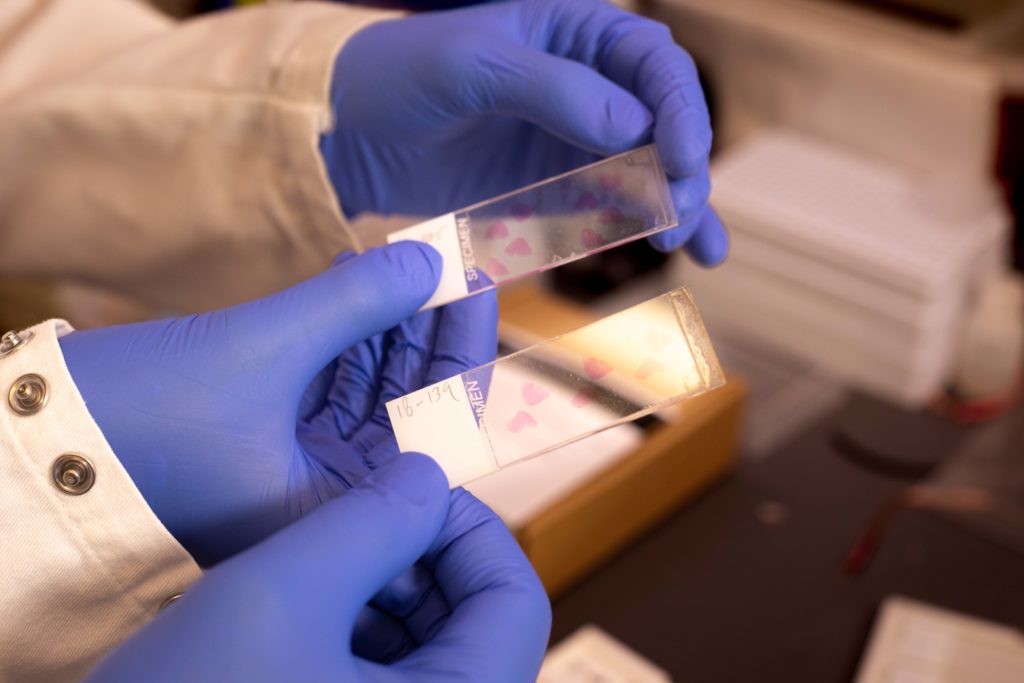
In the study, McNally and her collaborators took samples from patients with DSP-associated myocarditis, or a family history of myocarditis, and developed engineered heart tissues based on them. Investigators then compared immune reactions in heart tissues affected by myocarditis to those in healthy heart tissues and found that the myocarditis-affected heart tissues were hypersensitive to immune stimulation.
Additionally, the myocarditis heart tissues developed from patient cells lost function when placed under strain, according to the study.
By administering drugs designed to soothe inflammation and the immune response, investigators were able to return heart tissues affected by myocarditis to normal contractile function. Similarly, medications designed to rescue DSP function reduced inflammatory biomarkers of myocarditis, according to the study.
The findings paint a more detailed picture of how heart muscles function in myocarditis, McNally said.
“We found that the heart tissues themselves had an increase in innate immune activation, a signature of myocarditis, but they did so in the absence of immune cells, suggesting the heart cells themselves participate in this process,” McNally said.
Next, McNally and her collaborators plan to turn their attention to testing various drugs to improve myocarditis heart tissue function in the hopes of developing new therapies for the condition.
“We’re very excited about working with engineered heart tissues. It gives us the capacity to look at human cells in a human organoid context and now we can test all the different pathways that we discovered in these cells. There are drugs that can target these pathways, and we can use specific drugs directed right at these pathways,” McNally said. “Hopefully, we will be able to prevent these individuals from having additional bouts of myocarditis and going on to develop heart failure.”
Daniel Selgrade, a student in Feinberg’s Medical Scientist Training Program (MSTP) was first author of the study. Dominic Fullenkamp, ’14 MD, ’12 PhD, ’15, ’16 GME, assistant professor of Medicine in the Division of Cardiology; and Ivana Chychula, a member of the McNally laboratory, were co-authors of the study.
The study was supported by National Institutes of Health grants HL128075, HL167813, HL162454, HL163392, AR43380 and HL134633. Additional funding was provided by the Leducq TransAtlantic Foundation, the International Institute for Nanotechnology at Northwestern University, the Chicago Biomedical Consortium and an equipment grant from the National Institutes of Health (S10OD026867).
Myocarditis and COVID-19
Myocarditis garnered newfound attention during the COVID-19 pandemic, McNally said.
People infected with COVID-19 are more likely to develop myocarditis, which has also emerged as a symptom of long COVID, according to the American Heart Association.
“First and foremost, we learned that myocarditis was increased by being exposed to the COVID-19 virus itself, so COVID can cause myocarditis,” McNally said. “Then it got even more attention when we discovered that there was an increase in myocarditis in individuals who were receiving vaccines, particularly young men.”
The findings of McNally’s latest study put more focus on heart muscles themselves, as opposed to immune cells, which were traditionally thought to kickstart inflammatory responses in myocarditis.
“Most people think of myocarditis as having to do with the immune cells that come into the heart and cause all sorts of trouble and inflammation,” McNally said. “It was quite interesting to see that the heart cells themselves had this increased inflammation.”






