The failure of lung epithelial cells to complete transition from a stem cell-like state into a fully differentiated state causes lung fibrosis, according to a Northwestern Medicine study published in Proceedings of the National Academy of the Sciences (PNAS).
Administering a small molecule to mice with lung fibrosis helped complete this cellular transition in both young and old mice, suggesting it could become part of therapy in the future, according to Alexander Misharin, MD, PhD, assistant professor of Medicine in the Division of Pulmonary and Critical Care and co-senior author of the study.
“Currently, therapeutic options for patients with pulmonary fibrosis are limited to lung transplantation and two drugs with modest efficacy and severe side effects, so new drugs that could slow down progression or revert pulmonary fibrosis are much needed,” Misharin said.
Pulmonary fibrosis is a condition in which lung tissue becomes damaged and scarred, gradually and irreversibly eroding lung function. Misharin and his collaborators examined cells in the lung epithelium, including flat type 1 epithelial cells, which are involved in gas exchange between the lung alveoli and the blood, and cuboidal type 2 cells, which normally produce surfactant.
If type 1 cells are injured and die — which inevitably happens over a lifetime — type 2 epithelial cells undergo a transformation, dividing and differentiating into type 1 cells to replace those that are lost.
“They act as makeshift stem cells,” said Misharin.
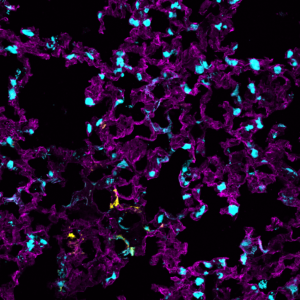
In young animals these epithelial cells eventually complete this transition, and experimental lung fibrosis in young mice is usually self-resolving. In older animals, however, these type 2 cells can become “stuck” in this transition process, either dying or lingering as alveolar epithelial progenitor cells. If the transitionary cells die, the initial lung injury remains unresolved and this process repeats. If the cells instead get stuck in transition, they can drive recruitment of immune cells and send signals that activate fibroblasts.
“Acting together, these cell types drive increased deposition of extracellular matrix, leading to the development of lung fibrosis,” Misharin said.
This transition process is stressful for epithelial cells and while cells from young animals can handle the pressure, cells from old animals often fail — part of why pulmonary fibrosis is more common in older adults.
In the current study, the authors demonstrated that a small molecule called ISRIB can help. The molecule, which is known to aid protein translation, shepherded type 2 epithelial cells through their transition into type 1 cells, accelerating epithelial repair and thus alleviating lung fibrosis. Importantly, it was effective in both young and old animal models, according to the study.
“These cells reshape and change everything they do; it’s like moving into a different country and starting a new job, which can be very stressful,” Misharin said. “This drug can help them complete this transition.”
Similar small molecules targeting stress pathways are currently entering clinical trials for other conditions, and Misharin said that as long as they are deemed safe, they could be tested in human patients to slow progression of pulmonary fibrosis. There are other applications as well, including in treating persistent lung damage caused by COVID-19, according to Scott Budinger, MD, the Ernest S. Bazley Professor of Airway Diseases, chief of Pulmonary and Critical Care in the Department of Medicine and co-senior author of the study.
“We found a similar population of transitioning epithelial cells that were targeted by ISRIB in mice in the lungs from our patients with severe COVID-19 lung damage who have required lung transplantation,” said Budinger, who is also a professor of Cell and Developmental Biology, referring to a recent study published in Science Translational Medicine. “This suggests that drugs like ISRIB might promote repair in patients with persistent lung scarring after COVID-19.”
Satoshi Watanbe, PhD, former postdoctoral fellow in the Division of Pulmonary and Critical Care and now an assistant professor of Respiratory Medicine at Kanazawa University Graduate School of Medical Sciences, was lead author of the study. Co-authors of the study include Cara Gottardi, PhD, associate professor of Medicine in the Division of Pulmonary and Critical Care and director of the Walter S. and Lucienne Driskill Graduate Program in Life Sciences (DGP); Manu Jain, MD, professor of Medicine in the Division of Pulmonary and Critical Care and of Pediatrics; Richard Morimoto, PhD, professor in the Ken and Ruth Davee Department of Neurology; Jacob Sznajder, MD, the Ernest S. Bazley Professor of Asthma and Related Disorders, professor of Medicine in the Division of Pulmonary and Critical Care and of Cell and Molecular Biology; and Paul Reyfman, MD, ’17 GME, assistant professor of Medicine in the Division of Pulmonary and Critical Care.
Budinger, Gottardi and Misharin are members of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
This study was supported by National Institutes of Health grants ES013995, HL071643, AG049665, HL135124, HL153312, AG049665, AI135964 and K08HL146943; Northwestern University’s Lung Sciences Training Program 5T32HL076139-13; and The Veterans Administration Grant BX000201.