Northwestern Medicine investigators have uncovered a novel pathogenic mechanism used by the bacterium Pseudomonas aeruginosa to promote more severe infections, according to a recent study published in the Proceedings of the National Academy of Sciences.
“The novelty of this is that Pseudomonas aeruginosa’s contact-dependent growth inhibition system, which had been discovered as a factor that is fairly widespread in bacteria and allows bacteria to compete against other bacteria, could also act as a virulence factor and enhance infection severity,” said Alan Hauser, MD, PhD, vice chair of the Department of Microbiology-Immunology and professor of Medicine in the Division of Infectious Diseases.
Pseudomonas aeruginosa is a common bacterium found in the environment, including soil and water, but can also cause serious infections in patients who are hospitalized or immunocompromised.
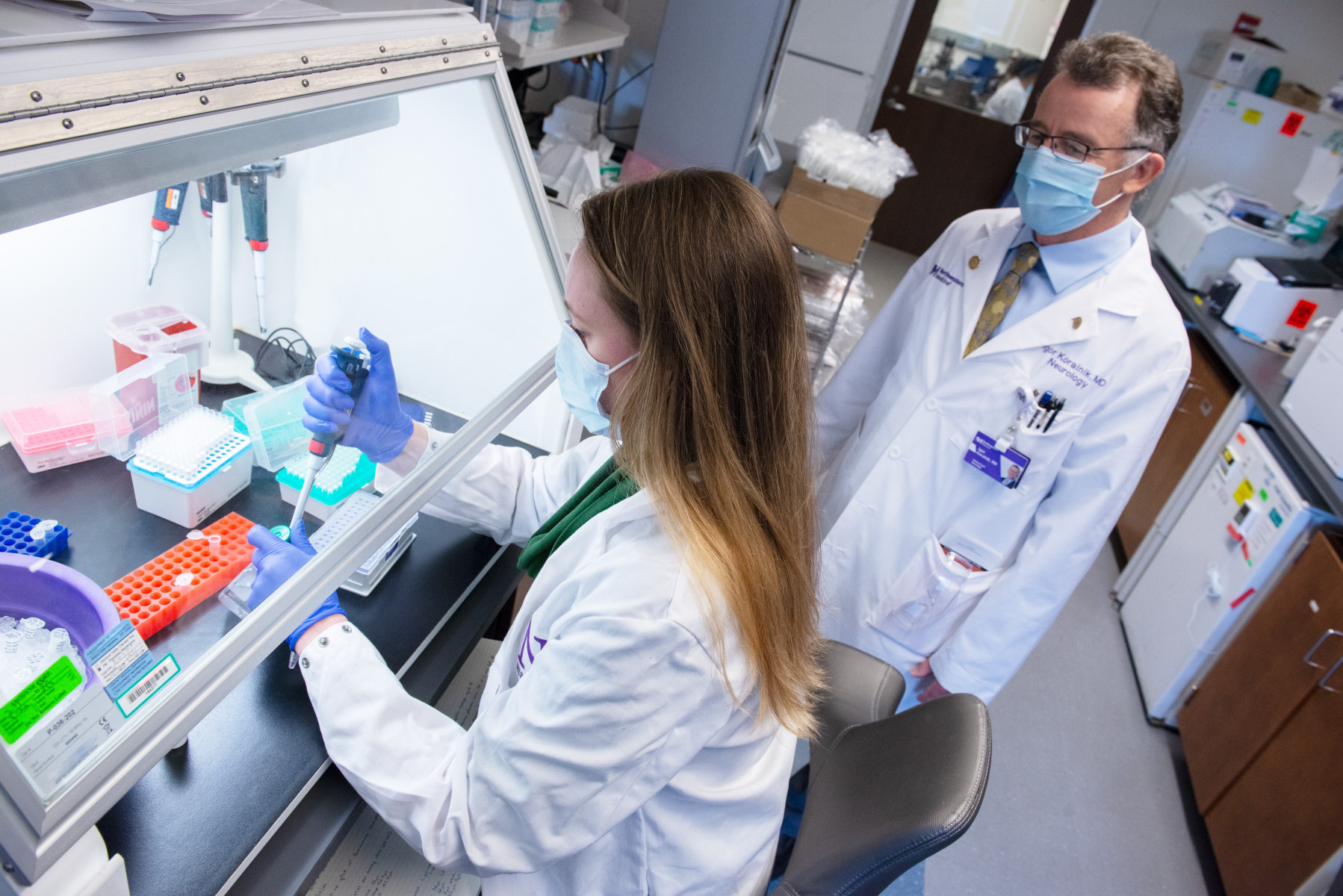
For the current study, the investigators analyzed 100 Pseudomonas aeruginosa strains from blood samples of hospital patients who were diagnosed with bloodstream infections. These strains were then inoculated into mice, allowing the investigators to determine each strain’s level of virulence, or aggressiveness.
“What we found was surprising in that for some of these strains as few as three million bacteria was sufficient to cause a severe illness in a mouse, whereas other strains required three billion bacteria,” Hauser said — a thousand-fold difference.
According to Hauser, this suggested that Pseudomonas aeruginosa’s accessory genome, which are genes found in some strains but not others, may be responsible for the varying levels of virulence between strains.
Using a comparative genomics approach, the investigators sequenced the genomes of all 100 Pseudomonas aeruginosa strains and compared their accessory genomes. This analysis revealed that a number of accessory genes were overrepresented in the high virulence strains. Approximately two-thirds of these were then shown to enhance the aggressiveness of Pseudomonas aeruginosa.
Going one step further, the investigators studied the mechanism of one of the identified genes, called CdiA.
“This gene was really interesting because similar genes have been found in other species of bacteria and have been shown to play an important role in the ability of bacteria to compete against one another,” Hauser said.
During this competitive process, called contact-dependent growth inhibition, the poisonous tip of a stalk located on the bacterium’s surface makes contact with other bacterial cells, piercing it and killing it.
With the help of Karla Satchell, PhD, director of the Center for Structural Genomics of Infectious Diseases and professor of Microbiology-Immunology, the investigators determined that the poisonous tip of the CdiA gene was an enzyme that cleaves transfer RNAs purified from both bacteria and mammalian cells.
“That suggested that maybe there’s a conserved mechanism here — that in the same way these bacteria killed other bacteria, they may also be able to kill mouse cells or potentially human cells,” Hauser said.
In the long term, Hauser said he hopes their findings may be used to develop a diagnostic test to predict the severity of illness for those patients diagnosed with Pseudomonas aeruginosa infections.
“We’re currently working on a project in which we use machine learning to look at genomes of Pseudomonas aeruginosa and from that genomic information predict which strains are high virulence and which are low virulence,” Hauser said.
This work was funded by the National Institutes of Health grants HHSN272201700060C, F32 AI108247, R01 AI118257, R01 AI053674, U19 AI135964, K24 AI04831, and R21 AI129167.