Northwestern Medicine scientists have identified a gene, called isocitrate dehydrogenase 3-alpha, that promotes glioblastoma tumor growth, according to a study published in Science Advances.
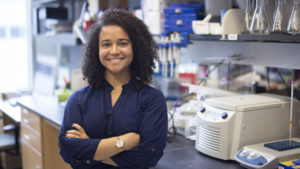
A drug that targets this gene could be a new therapy for this common yet aggressive form of brain cancer, said Alexander Stegh, PhD, associate professor in the Ken and Ruth Davee Department of Neurology in the Division of Neuro-oncology, and senior author of the study. Jasmine May, a seventh-year student in the Medical Scientist Training Program, was the first author.
Glioblastoma (GBM) are malignant tumors that can grow quickly, nourished by the ample blood supply in the brain. According to Stegh, they are particularly deadly, often materializing as high grade tumors as soon as they form.
Isocitrate dehydrogenase (IDH) are a group of enzymes that help regulate energy production processes in the mitochondria. Previous work in the Stegh laboratory had identified up-regulation of a non-mutated, wild-type form of IDH1 as a marker for brain tumor progression that is highly expressed in GBM, piquing their interest.

“That study motivated us to fully understand the impact of all IDH family members on GBM progression,” said Stegh, also a professor of Medicine in the Division of Hematology and Oncology and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
In the current study, Stegh and his collaborators looked at the third variant, isocitrate dehydrogenase 3-alpha (IDH3A), the catalytic subunit of the IDH3 enzyme. They first examined IDH3A levels in a large database of genetic data from GBM tumors, and in GBM tumors resected from Northwestern patients. The scientists found IDH3A was expressed at much higher levels in patient tumors than in normal brain tissue.
They then tested its function in mice, either over- or under-expressing IDH3A in patient-derived tumor cells. They found that elevated levels of IDH3A promoted GBM progression and those mice had shortened survival when compared to mice with decreased levels of IDH3A.
“In particular, we found that IDH3A inactivation was associated with a shift from a grade IV to grade III malignancy, indicating that inactivation of IDH3A reduces malignancy characteristics of GBM tumors,” Stegh said.
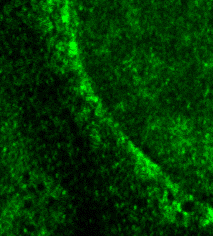
To unravel the molecular mechanisms at play, the scientists used microscopy, metabolomics and mass spectrometry studies to assess IDH3A subcellular distribution, binding partners, and functional effect on tumor cell metabolism. Surprisingly, they found IDH3A was gravitating towards the nucleus of the cell, binding to and regulating another enzyme called cytosolic serine hydroxymethyltransferase (cSHMT).
“By modulating cSHMT activity, IDH3A promotes the synthesis of nucleotides, the building blocks of DNA,” Stegh said. “We conclude that this non-canonical activity of IDH3A allows rapidly dividing GBM tumor cells to increase DNA synthesis to support cell division and unabated growth.“
This opens the door to a new therapeutic approach: targeting the IDH3A-cSHMT interaction.
“This could reduce the ability of tumor cells to synthesize DNA,” Stegh said. “Inhibition of DNA synthesis in turn is expected to reduce the growth of highly proliferative cancer cells.”
However, further investigation of the precise mechanisms underlying this interaction is required. Next, Stegh and his colleagues plan to examine the exact binding interface between IDH3A and cSHMT, and how the structures are altered once they form a complex.
“This information will be critical for identifying drugs that can disrupt the interaction between IDH3α and cSHMT,” Stegh said.
Other Northwestern co-authors include Foteini Kouri, PhD, research assistant professor of Neurology in the Division of Neuro-oncology; Lisa Hurley, senior research technologist in the Stegh laboratory; Serena Tommasini Ghelfi; Yanrong Ji, third-year student in the Driskill Graduate Program in Life Sciences; Peng Gao, PhD, research assistant professor of Medicine in the Division of Hematology and Oncology; Andrea Calvert, PhD, postdoctoral fellow in the Stegh laboratory; Navdeep Chandel, PhD, the David W. Cugell, MD, Professor of Medicine in the Division of Pulmonary and Critical Care and of Cell and Molecular Biology; Ramana Davuluri, PhD, professor of Preventive Medicine in the Division of Health and Biomedical Informatics and Craig Horbinski, MD, PhD, associate professor of Pathology and of Neurological Surgery.
Chandel, Davuluri and Horbinski are also members of the Lurie Cancer Center.
This research was supported by the Center for Cancer Nanotechnology Excellence Initiative of the National Institutes of Health (NIH), under awards U54 CA151880, 199091 and R01CA208783. Other NIH grants include T32 CA09560, T32 GM008152, R01CA193256, P30CA014236, R01LM011297 and R35CA197532. The study was also supported by the brain tumor SPORE grant P50CA221747.






