Overexpression of a protein called CHAF1B, which normally helps renew and replenish blood cells, could contribute to the development of leukemia, according to a Northwestern Medicine study published in Cancer Cell.
Therefore, reducing CHAF1B activity to normal levels may be a promising treatment for this deadly cancer, said Andrew Volk, PhD, a postdoctoral fellow in the Crispino laboratory and lead author of the study.
“You don’t have to get rid of it completely, just interfere with its ability to interact with other proteins,” Volk said.
John Crispino, PhD, the Robert I. Lurie, MD, and Lora S. Lurie Professor of Medicine in the Division of Hematology and Oncology and of Biochemistry and Molecular Genetics, was the senior author of the study.
Blood is one of the fastest-growing tissues in the body: The average adult produces over 2 million new red blood cells every second. These new blood cells are formed beginning with a process called self-renewal; stem cells divide in two, creating one new stem cell and one progenitor cell. The progenitor cell will eventually differentiate into a red blood cell, while the stem cell remains flexible, ready to divide again.
The study authors discovered that CHAF1B plays a key role in ensuring the new stem cells retain their flexibility during this process.
“Without CHAF1B, the stem cells don’t self-renew and instead divide into two progenitor cells, which will eventually divide into four, and so on,” Volk said. “The blood functions normally until there’s no more stem cells left, which is termed exhaustion.”
Issues with differentiation can also lead to some cancers, according to Volk. Progenitor cells can become “stuck” midway between stem cells and differentiated blood cells, and instead of carrying out their respective functions throughout the body, these leukemic blast cells end up consuming valuable nutrients and crowding out other, more useful cells.
In the current study, Crispino, Volk and collaborators found that CHAF1B was upregulated in multiple types of blood and solid tumor cancers. In fact, the level of up-regulation corresponded with the cancer’s severity: later stage cancers had higher levels of CHAF1B.
This may indicate that when overproduced, CHAF1B does its job too well, keeping blood cells from differentiating properly and causing cancer, according to the study. However, treating these leukemias is notoriously difficult; the constant cell division in blood means therapies that attack cancer cells directly tend to fade and become less effective over time.
“Every time the cells divide, they have the opportunity to incorporate mutations and change a little bit,” Volk said. “If you put pressure on that tumor, by way of a chemotherapy drug that starts killing the cells, then you’re going to put Charles Darwin in the driver’s seat and the cells are going to try and change to get around that.”
Instead, a therapy that corrects this improper differentiation could be much more useful, according to Crispino.
“Targeting CHAF1B may provide a true form of differentiation therapy, whereby leukemia cells are eliminated through forced maturation,” he said. “The beauty of this approach is the potential therapeutic window whereby targeting CHAF1B would have a selective effect on tumor cells.”
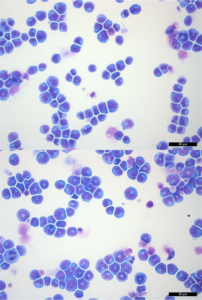
In the current study, the scientists generated mice using the Cre-Lox system, allowing them to selectively delete CHAF1B in the blood cells of live mice. They found that mice with both copies of CHAF1B deleted did not survive, but deleting just one copy was enough to suppress leukemic blast formation by allowing proper cell differentiation while maintaining normal blood cell function.
The scientists also examined the gene’s effects in human acute myeloid leukemia cell lines derived from patient samples, using CRISPR-Cas9 gene editing to prevent CHAF1B from being expressed. As in mice, they found that differentiation increased and tumor formation was reduced.
While CRISPR is useful in experimentation, it’s not yet viable as a patient therapy. With an eye towards the clinic, the authors expressed a CHAF1B inhibitor protein that binds with CHAF1B and prevents it from functioning, and tested the new inhibitor’s efficacy in mice, finding that it blocked tumor formation.
“We found that you don’t actually need to reduce the amount of CHAF1B — you don’t need to knock down genes, use CRISPR or do anything invasive,” Volk said. “All you need to do is prevent CHAF1B from interacting with its partners, then the mice don’t die from cancer.”
The next step towards a human treatment is developing a small-molecule drug that mimics this inhibitor, according to Volk.
“Something like this would have very little effect in healthy cells,” Volk said. “The ultimate goal would be to develop a drug that you could even ingest orally — a drug like that could have a huge impact on patients.”
Other Northwestern co-authors include Ali Shilatifard, PhD, the Robert Francis Furchgott Professor, chair of Biochemistry and Molecular Genetics, director of the Simpson Querrey Center for Epigenetics and a professor of Pediatrics; Elizabeth Bartom, PhD, assistant professor of Biochemistry and Molecular Genetics; Kaiwei Liang, PhD, a postdoctoral fellow in the Shilatifard laboratory; Praveen Suraneni, PhD, a postdoctoral fellow in the Crispino laboratory; and Stacy Marshall, lab manager in the Shilatifard laboratory.
Crispino and Shilatifard are also members of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
The study was supported by the Samuel Waxman Cancer Research Foundation, National Institutes of Health (NIH) grants R01 CA101774 and T32 CA080621, a Scholar Award from American Society of Hematology, National Cancer Institute (NCI) grants R35 CA197569 and R50 CA221848, the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Northwestern University Pathology Core and Flow Cytometry Facilities funded by NCI CA060553, and cell sorting was performed on a BD FACSAria SORP system purchased with the support of NIH 1S10OD011996-01.






