A protein found to interfere with the molecular defense network in place to kill cancer cells could mark a turning point in the way physicians treat brain tumors in the future.
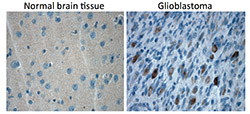
Alexander Stegh, PhD, assistant professor of Neurology and Medicine, and colleagues at the Northwestern Brain Tumor Institute have discovered the role Bcl2L13 plays in protecting glioblastoma multiforme (GBM) from apoptosis, or cell death, during treatment.
Despite significant advances in neurosurgical techniques, radiation oncology and numerous clinical trials, high-grade brain tumors, in particular GBM, remain incurable. GBM is the most common and aggressive form, with an average life expectancy of just 12-15 months.
“We identified Bcl2L13 as an anti-apoptotic protein that is overexpressed, not only in GBM, but in other systemic and solid malignancies,” said Stegh, a member of the Robert H. Lurie Comprehensive Cancer Center. “The protein promotes tumor growth in vivo and we were able to identify specific enzymes that it directly interacts with.”
The findings were recently published in Proceedings of the National Academy of Sciences.
To determine how Bcl2L13 is protecting cancer cells, scientists first explored potential protein-protein interactions. The screening uncovered a pair of enzymes (ceramide synthases 2 and 6) that produce ceramides, a major building block of the cell membrane that are responsible for protecting the cell’s internal components from the external environment. Enzymes are proteins that act to accelerate metabolic reactions.
“Importantly, ceramides are not purely structural elements, but represent important messenger molecules that are part of many signaling cascades within a cell,” Stegh said. “In particular, ceramides can activate a variety of proteins that trigger the death of tumor cells.”

When Bcl2L13 is overexpressed, it binds to ceramide synthases and blocks their ability to generate ceramides. The reduced activity of ceramide synthases and lower ceramide levels are correlated with shorter survival time for cancer patients.
“This is the first time that ceramide synthase activity has been shown to be directly regulated by a Bcl2 family protein and establishes the Bcl2L13-ceramide synthase interaction as a target for potential therapy,” Stegh said. “Despite the importance of ceramides in slowing cancer progression, efforts to use it therapeutically have not been successful.”
Stegh points to pharmacological neutralization of Bcl2L13 as a way to increase ceramide levels to trigger ceramide-mediated apoptosis.
His lab will attempt to determine the exact binding site of Bcl2L13 and ceramide synthases in an effort to determine how best to design drugs that can inhibit the interaction.
“Another ongoing extension of this work will be conducted with our Northwestern Medicine collaborators to design spherical nucleic acids – gold nanoparticles – that specifically target Bcl2L13,” Stegh said. “The goal is to knockdown Bcl2L13 expression in tumors to promote ceramide production and trigger cancer cell death.”
The study was funded by a grant from the Illinois division of the American Cancer Society, the Dixon Translational Research Grants Initiative of the Northwestern Memorial Foundation, the James S. MacDonnel 21st Century Initiative and the Coffman Charitable Trust.






