Northwestern Medicine scientists have discovered a new gene and revealed its role in the body’s inflammatory response against infection.
“In today’s scientific climate it’s not common to make a discovery like this because the human genome has been largely mapped,” said Christian Stehlik, PhD, John P. Gallagher Research Professor of Rheumatology. “Somehow, this gene and the protein it encodes had been overlooked.”
The work by Stehlik and colleagues may provide a new therapeutic target against inflammatory responses produced when the body recognizes foreign DNA from a virus like HIV, or when it attacks itself in autoimmune diseases such as Systemic lupus erythematosus, inflammatory myocarditis or Aicardi-Goutières syndrome. The findings were published on Feb. 16 in Nature Immunology.
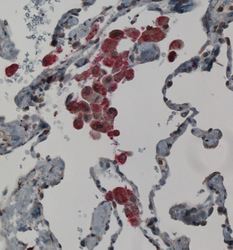
The project focused on how the sensors responsible for detecting viruses and triggering defensive inflammatory responses, known as inflammasomes, are controlled. The scientists found that the protein, named POP3, interferes with the proper assembly of these sensors.
“This regulation is important to limit the accelerated host responses that lead to autoinflammatory and autoimmune disease,” said Stehlik, a member of the Interdepartmental Immunobiology Center and the Robert H. Lurie Comprehensive Cancer Center. “POP3 is the first inhibitor identified that targets this pathway.”
Using a unique POP3 mouse model, Stehlik was able to observe the effects of expressing the protein, which is normally not found in mice. The in vivo findings were similar to those in human cells. They showed that elevated levels of POP3 dampen inflammation as well as anti-viral responses, suggesting that the protein may be a useful tool in the development of new anti-inflammatory or antiviral drugs.

“Factors that promote a balanced inflammasome response are essential for maintaining homeostasis, because weakened or overly strong inflammatory responses are detrimental to the body,” said Stehlik, who worked closely with Andrea Dorfleutner, PhD, and Sonal Khare, PhD, both research assistant professors of Medicine-Rheumatology. “We now know that POP3 is helping to control this double-edged sword.”
Two recent studies in Nature and Science have shown that HIV triggers this same pathway, causing uncontrolled inflammation and T-cell death.
“It’s highly speculative, but if you had a protein that inhibits this pathway, it might actually be able to prevent the progression of HIV,” Stehlik said.
Stehlik believes a more plausible pursuit will be to introduce more POP3 to help prevent autoimmune disease, since there is some evidence that this pathway is excessively active in lupus. He plans to conduct a follow-up study to determine if a small molecule that mimics POP3 can be used in this capacity.
“Based on our previous work, I think this proof-of-principle study will likely be successful,” Stehlik said. “The challenge will be to design a molecule that acts like the protein and then get it into these specific white blood cells.”
The work was supported by National Institutes of Health grants GM071723, HL097183, AI092490, AI082406, AI099009 and AR064349, a Cancer Center Support Grant CA060553, a Skin Disease Research Center grant AR057216 and an American Heart Association grant 12GRNT12080035.
The Stehlik lab worked in collaboration with Harris Perlman, PhD; Carla Cuda, PhD; Alexander Misharin, MD, PhD; and Eva Gottwein, PhD, at Feinberg, as well as David Greaves, PhD, at the University of Oxford and John Reed, MD, PhD, at Hoffman-La Roche AG.






