Investigators were able to halt the growth of glioblastoma, an aggressive form of brain cancer, by inhibiting an enzyme called CDK5, according to a Northwestern Medicine study published in Cell Reports.
The discovery of this enzyme’s regulatory influence on glioblastoma may open the door to a long-awaited improvement upon current therapy options, according to Subhas Mukherjee, PhD, research assistant professor of Pathology and first author of the study.
“The mortality rate for glioblastoma has only moderately changed in last thirty years,” Mukherjee said. “The current drug, temozolomide, is somewhat effective when the tumor recurs — and one of the major problems with glioblastomas is they tend to come back.”
CDK5 is a protein kinase, a class of enzymes that modify the function of proteins and play a major role in protein and enzyme regulation. While CDK5 was previously known to be associated with neurodegenerative disorders including Alzheimer’s disease, its involvement with glioblastoma has only been recently documented, according to Mukherjee.
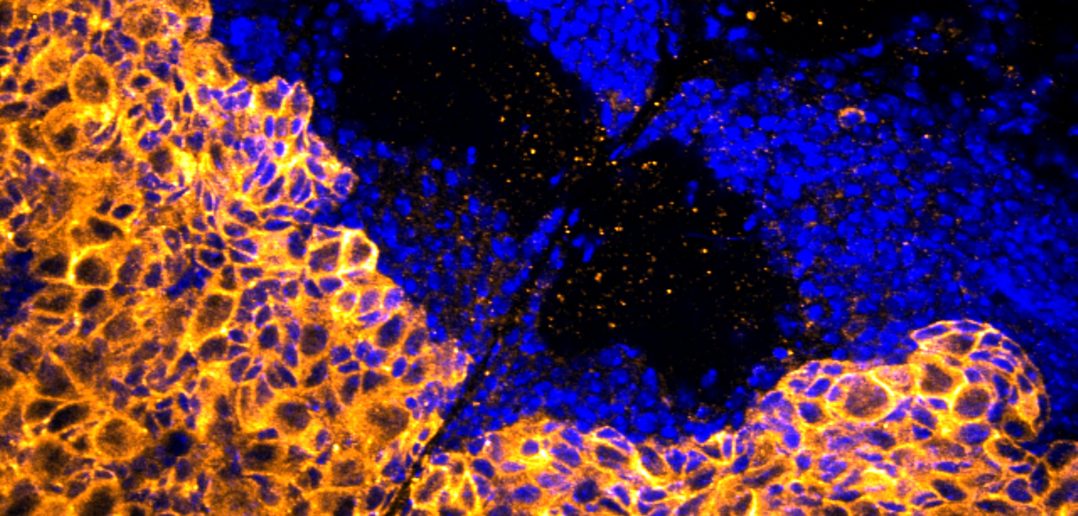
Glioblastoma’s high likelihood of recurrence is driven in part by glioma stem cells, self-renewing cancer stem cells that support the growth of tumors. Mukherjee, who has been investigating these glioma stem cells since he was a postdoctoral fellow at Emory University, conducted a gene screen on Drosophila models with brain tumors against 29 separate models, each with a single gene silenced.

Mukherjee and his collaborators found the flies’ tumors shrunk and the number of cancer stem cells decreased after silencing the gene that coded for CDK5. In humans, they found a large number of patients with glioblastoma also had high levels of the enzyme, after analyzing glioblastoma patient genetic data in The Cancer Genome Atlas, a database of genetic data from 11,000 cancer patients sponsored by the National Institutes of Health (NIH).
“We started running tests in our lab and found CDK5 promotes a high level of stem-ness in cells, so they proliferate and grow more,” Mukherjee said. “We isolated the cells that were most stem-like, and found that they have a high level of CDK5 compared to ones that are less stem-like.”
With the growth-regulating properties of CDK5 established, investigators then applied an experimental CDK5 inhibitor to human glioblastoma cells, finding it stopped tumor growth and caused cancer stem cells to behave less stem-like, losing some of their self-renewal ability.
In addition, they discovered only two of the three main classifications of glioblastoma have highly expressed CDK5, which suggests patients with the third subtype — mesenchymal glioblastoma — might not see the same benefit.
The authors note that the reduction of stem-ness, combined with the drug’s specificity and ability to cross the blood-brain barrier, make it an excellent candidate for a therapy. In fact, Mukherjee is currently working with Northwestern’s Center for Molecular Innovation and Drug Discovery to create an improved, homegrown version of the drug.
“We will hopefully generate some models and start testing within a few months,” Mukherjee said.
Mukherjee predicts that the future treatment might function as a first-line treatment option in coordination with chemotherapy. Preliminary data suggests that CDK5 is central to tumor recurrence, so a CDK5 inhibitor might conceivably function in two ways — stopping tumors from growing and preventing them from coming back.
“The idea is to kill the remnants and glioma stem cells after chemotherapy,” Mukherjee said. “Those are the cells that persist and cause recurrence.”
Daniel Brat, MD, PhD, chair and Magerstadt Professor of Pathology, was senior author of the study. Read a Northwestern Medicine magazine profile of his work spearheading transformations in the field of pathology, or listen to Brat on an episode of Feinberg’s Breakthroughs Podcast.
This study was supported by NIH grants R01 CA176659, CA149107 and K25CA181503; the Winship Cancer Institute National Cancer Institute Cancer Center Support Grant P30CA138292 and the Georgia Research Alliance.






