Northwestern Medicine scientists have discovered a novel mechanism that could be responsible for aiding the spread of one of the most common sexually transmitted diseases (STD) in America.
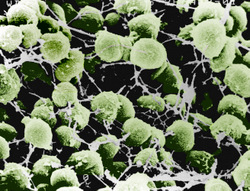
Investigators used a synthetic barrier to study the ability of N. gonorrhoeae, the bacterium responsible for gonorrhea, to spread infection. When exposed to seminal plasma, the liquid part of semen, 24 times more bacteria were able to move through the barrier.
“This suggests for the first time that seminal plasma may have a direct role in promoting transmission of a sexually transmitted infection,” said principal investigator Hank Seifert, PhD, John Edward Porter Professor of Biomedical Research. “Although we cannot directly test whether seminal plasma enhances transmission without an animal model, the enhanced capabilities revealed in our studies are consistent with that hypothesis.”
The findings were published in mBio. Mark Anderson, PhD, a postdoctoral fellow in the Seifert lab was first author.

Gonorrhea is an STD that infects an estimated 100 million people annually worldwide. The infection is transmitted from person to person through sexual contact. If untreated, it can lead to serious and permanent health problems, including pelvic inflammatory disease in women and epididymitis in men. The Centers for Disease Control estimates 800,000 new cases occur in the United States every year.
“Our work characterizing the mechanisms of this disease and its transmission are vital for the development of new prevention strategies,” said Seifert, professor of Microbiology-Immunology and a member of the Center for Genetic Medicine, Interdepartmental Immunobiology Center and Robert H. Lurie Comprehensive Cancer Center.
That’s in large part because antibiotics once effective against gonorrhea, including penicillin, are no longer recommended due to bacterial resistance to these drugs.
A second study finding revealed that exposure to seminal plasma enhanced the formation of bacterial microcolonies on epithelial cells. These cells line the body cavities where bacteria establish infection. The formation of microcolonies allows the bacteria to resist the natural flow that can dislodge them. This, in-turn, helps them remain attached at the site of infection.
The work was done in collaboration with Berenike Maier, PhD, at the University of Cologne in Germany and was supported by National Institutes of Health grants R37 AI033493 and R01 AI044239, and a grant from the German Research Foundation.






