Immunotherapy administered before and after chemotherapy along with surgical removal of the bladder improved survival compared to chemotherapy alone in patients with muscle-invasive bladder cancer, according to results of a recent clinical trial published in the New England Journal of Medicine.
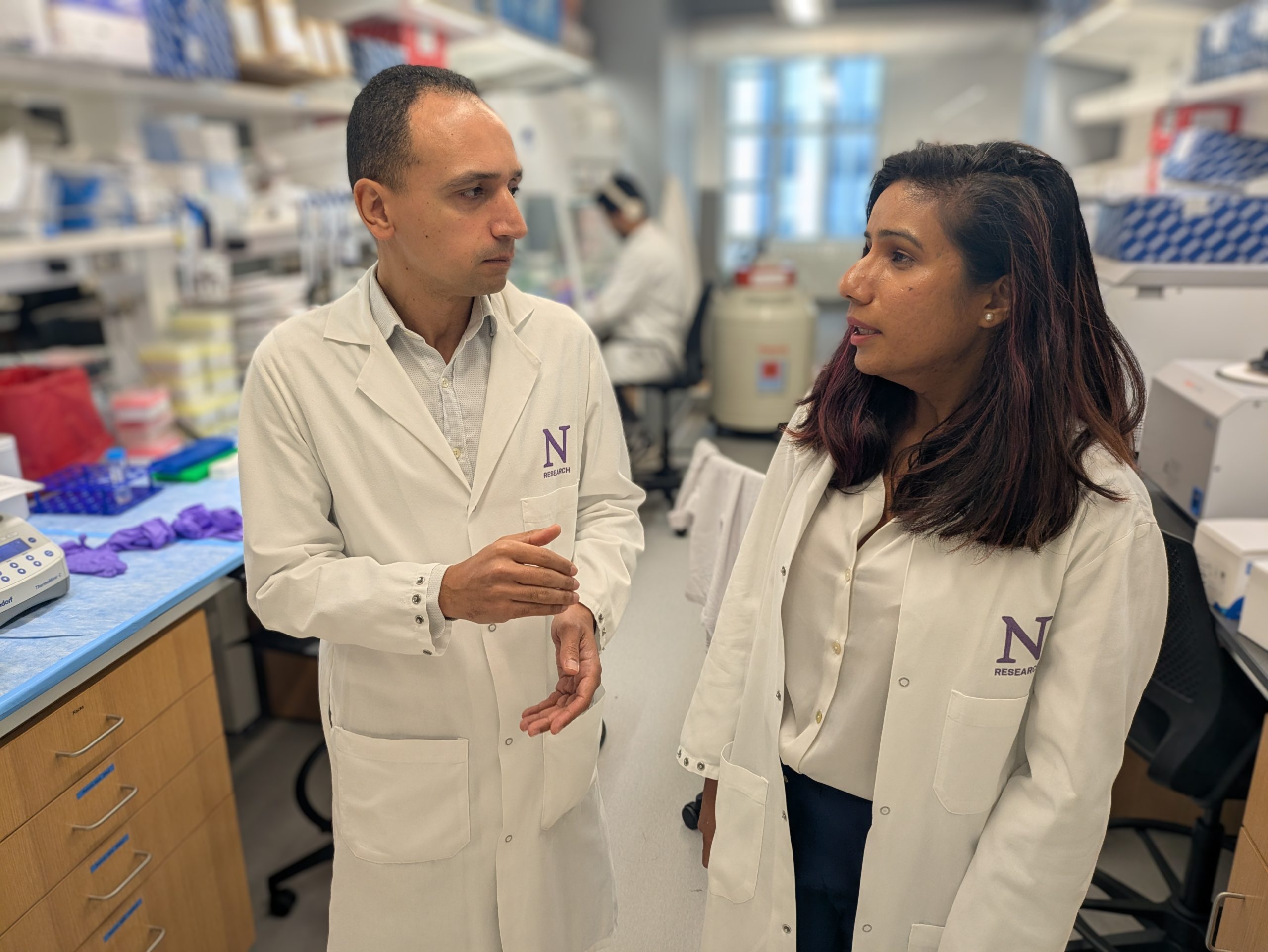
The findings demonstrate the potential of a new treatment regimen for patients with locally advanced bladder cancer, according to Joshua Meeks, ‘03 MD, ‘05 PhD, ‘06, ‘11 GME, the Edward M. Schaeffer, MD, PhD Professor of Urology and a co-author of the study.
“This is the first trial that’s shown that you can add immunotherapy to chemotherapy and show improved response and a survival benefit,” said Meeks, who is also a professor of Biochemistry and Molecular Genetics and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “This is very likely to become the new standard of care.”
For more than 20 years, the standard of care for advanced bladder cancer (stages II to III) involved chemotherapy followed by radical cystectomy, or surgical removal of the bladder and surrounding lymph nodes. However, approximately half of patients experience recurrence within three years after treatment.
“These patients have the most to lose or gain, so that’s why we treat them more aggressively,” Meeks said. “What hasn’t been clear is if adding immunotherapy to chemotherapy has any benefit. In the metastatic setting, it has not been necessarily as successful.”
In the current clinical trial, more than 1,000 patients with localized bladder cancer at academic medical centers from 22 countries in Europe, Asia, North America, Australia and South America were enrolled.
Participants were randomized to receive durvalumab immunotherapy plus chemotherapy (gemcitabine and cisplatin) every three weeks for four cycles, then radical cystectomy followed by durvalumab every four weeks for eight cycles, or neoadjuvant chemotherapy followed by radical cystectomy alone.
After 24 months, follow-up analyses showed that event-free survival and overall survival was longer in the durvalumab group compared to patients who received chemotherapy with radical cystectomy alone.
In the durvalumab group, event-free survival was 67.8 percent and overall survival was 82.2 percent. In the chemotherapy with radical cystectomy group, event-free survival was 59.8 percent and overall survival was 75.2 percent. Treatment-related adverse events were also the same in both groups (41 percent).
The findings highlight a new treatment regimen for patients with advanced, muscle-invasive bladder cancer that improves treatment response and survival with minimal side effects, Meeks said.
“We have a new treatment that has a chance to improve response and survival for patients with muscle-invasive bladder cancer,” Meeks said. “For patients that want to aggressively fight this cancer, we have a new way to do that with a minimal increase in toxicity. Our next steps are to determine which tumors will benefit from the addition of durvalumab and why it is so effective for stage II to III bladder cancer, so we really have more work to do.”
David VanderWeele, MD, PhD, associate professor of Medicine in the Division of Hematology and Oncology and director of the Lurie Cancer Center’s OncoSET Precision Medicine Program, served as the local principal investigator for the NIAGRA trial at Northwestern Medicine.
This work was recently presented at the European Society for Medical Oncology’s 2024 Annual Meeting and was supported by AstraZeneca.