While the worldwide vaccination campaign is underway, continued spread of COVID-19 and the specter of long-term symptoms mean the pandemic is far from over. Northwestern Medicine scientists and clinicians have continued to investigate methods to combat the disease, including strategies to conduct clinical trials during a pandemic, studying neurologic symptoms in children and reflecting on the importance of professional medical organizations during a public health crisis.
Remote Research and Clinical Trial Integrity

The COVID-19 pandemic has been an enormous obstacle to clinical trial research: As of April 2021, the National Institutes of Health listed more than 1,700 suspended clinical trials. Ongoing trials that were not suspended also likely face challenges with enrollment and adherence to trial protocols that require in-person contact, requiring investigators to decide which procedures are worth conducting in-person, according to an editorial published in JAMA authored by Mary McDermott, MD, ’92 GME, the Jeremiah Stamler Professor and a professor of Medicine in the Division of General Medicine and Geriatrics.
“Investigators should be thoughtful about which measures and interventions can be performed accurately remotely, and which require in-person interactions to ensure integrity of the trial,” said McDermott, who is also a professor of Preventive Medicine in the Division of Epidemiology.
In McDermott’s experience with a trial recently published in JAMA, she and her collaborators were able to accomplish some tasks remotely, such as mailing physical activity monitors to patients, who wore them for a week before mailing them back to investigators. However, other procedures such as walking tests had to be performed onsite or at a patient’s residence.
These experiences have prompted some investigators to consider ways they can make trial participation easier for the subjects, according to McDermott.
“There are many advantages to having participants come to the medical center for some measures that cannot be collected safely or feasibly at home, such as treadmill stress testing or muscle biopsies” McDermott said. “On the other hand, having participants pick up study pill interventions every three months instead of every month is less burdensome for participants and just makes sense.”
Neurological Symptoms in Children

More than 20 percent of children hospitalized for acute COVID-19 or multisystem inflammatory syndrome had neurological symptoms, according to a study published in JAMA Neurology.
Symptoms were mostly resolved by the time of discharge, but a small subset of patients developed new neurologic disabilities or died. Further inquiry is required to identify which children may be at risk of neurological symptoms and how to effectively treat the conditions, according to Kelly Michelson, MD, MPH, the Julia and David Uihlein Professor of Bioethics and Medical Humanities, director of the Institute for Public Health and Medicine’s Center for Bioethics and Medical Humanities, and a co-author of the study.
“Understanding the extent to which children infected with SARS-CoV-2 also develop neurologic symptoms is crucial to determine how to support and treat children with new neurologic problems,” said Michelson, who is also a professor of Pediatrics in the Division of Critical Care.
In the multi-center trial studying nearly 1,700 patients aged 21 years or younger who were hospitalized with COVID-19, patients were classified as having neurologic involvement or not having neurologic involvement. Neurologic involvement included both acute neurologic disease (infection, demyelination or stroke) and acute neurologic signs or symptoms.
Patients with underlying neurological disorders were more likely to have COVID-19-related neurologic involvement. Among the patients with neurologic involvement, 12 percent had life-threatening conditions, including severe encephalopathy or stroke.
The wide range of neurologic conditions measured means studies like these will be vital for determining the extent and severity of neurological symptoms of COVID-19 in children, according to Michelson.
“The CDC should continue to fund efforts to follow these children over the next year or more so that we can understand the disease course for children with neurologic sequelae of SARS-CoV-2 infection,” Michelson said.
This study was funded by the U.S. Centers for Disease Control and Prevention under a contract to Boston Children’s Hospital.
American Heart Association: One Year of COVID-19

Despite the human toll of the pandemic, the clinical and scientific community rose to the challenge, according to Donald Lloyd-Jones, MD, the Eileen M. Foell Professor, chair of Preventive Medicine and lead author of an editorial published in Circulation.
In particular, the American Heart Association — of which Lloyd-Jones is the president-elect — rapidly funded dozens of studies examining the cardiovascular impacts of the then-mysterious disease. The organization also created a large national registry of hospitalized COVID-19 patients, which to date has data on 40,000 individual patients from hundreds of hospitals across the U.S.
“There were published results from this registry as early as November, illustrating the flexibility and nimbleness of an organization like AHA to contribute to public health crises rapidly and effectively,” said Lloyd-Jones, who is also a professor of Pediatrics and of Medicine in the Division of Cardiology.
However, the troubled U.S. response to the pandemic and the long tail of persistent COVID-19 symptoms are reminders that greater investment in public health infrastructure is needed — not just for pandemics, according to Lloyd-Jones.
“Most importantly, we have to improve the health of the public by preventing and controlling the chronic diseases such as obesity, diabetes and hypertension that put us at risk for more severe infection when there is a pandemic like this,” Lloyd-Jones said. “All hands are needed on deck!”
Disparate Impact of COVID-19 in Chicago

Black and Hispanic neighborhoods in Chicago experienced a markedly higher burden due to COVID-19, according to a Northwestern Medicine study published in the journal Health & Place.
Using data from the Cook County Medical Examiner, investigators demonstrated that neighborhoods on the Northwest, West and South sides of Chicago had higher mortality rates and years of potential life lost (YPLL) due to COVID-19.
“As researchers and clinicians, we need to be aware of the role of structural racism and discrimination play in health disparities,” said Sadiya Khan, ’09 MD, ’10 ’12 ’16 GME, assistant professor of Medicine in the Division of Cardiology and senior author of the study.
COVID-19 has disproportionately affected racial and ethnic minorities, but little work has focused on neighborhood-level impacts, according to the authors. Using addresses gleaned from death certificates, investigators used geo-spatial mapping to identify “hot” and “cold” spots where COVID-19 deaths per 100,000 were particularly high or low. In addition, the investigators compared premature mortality rates both before and after COVID for related census tracts.
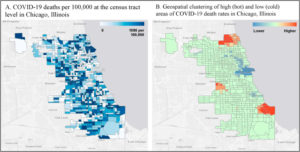
Hotspots with increased mortality and life-years lost were present on the far North, Northwest and South sides — coinciding with neighborhoods that have more Black and Hispanic residents. The wealthier North side of the city, with a largely white population, was the largest “cold” spot, providing a window into how neighborhood-level inequity contributes to large differences in public health outcomes, according to Khan.
“While much of the disparities have focused on difference by race or ethnicity, these reflect larger structural and systemic and structural vulnerabilities,” said Khan, who is also an assistant professor of Preventive Medicine in the Division of Epidemiology. “Research and health systems need to incorporate measures of social determinants of health, specifically structural racism and discrimination, to promote health equity and eliminate health disparities.”
This study was supported by NUCATS Institute grant KL2TR001424 from the National Institutes of Health National Heart, Lung, grant 19TPA34890060 from the Blood Institute and the American Heart Association, and a Sarnoff Cardiovascular Research Foundation Fellowship.
COVID-19 versus MIS-C

Clinicians can distinguish between severe COVID-19 and multisystem inflammatory syndrome in children (MIS-C) using disease presentation and organ involvement, according to a study published in JAMA.
The presentation of each disease can be similar, but these findings present an outline for determining the correct treatment, according to Bria Coates, MD, assistant professor of Pediatrics in the Division of Critical Care and a co-author of the study.
“This can improve our ability to anticipate complications, provide appropriate interventions, and counsel patients and families about prognosis,” Coates said.
MISC-C has broad diagnostic criteria, to increase suspicion for the syndrome and decrease the chance of missing cases. However, this means the diagnostic criteria overlaps with other diseases, including COVID-19, Coates said.
The study compared more than 1,000 patients under 21 years of age who were hospitalized with MIS-C or severe COVID-19. Patients with MIS-C were more likely than those with severe COVID-19 to be 6 to 12-years-old, be non-Hispanic Black, and have severe cardiovascular or mucocutaneous involvement and more extreme inflammation. Severity of respiratory symptoms did not distinguish between the two conditions, but isolated respiratory symptoms were more common in patients with COVID-19.
“As we get more experience with both diseases, comparing their presentations, trajectories and outcomes will help us develop more specific diagnostic criteria and ensure the right child is getting the right treatment,” Coates said.






