Northwestern Medicine scientists have discovered that a subset of laboratory-modified T-cells can promote the repair of lung tissue damaged by viral pneumonia, according to a recent study published in The Journal of Clinical Investigation.
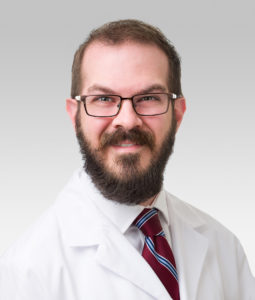
The findings suggest that the cells, called induced regulatory T-cells, or iTregs, may have potential as a cellular therapy for treating viral pneumonia-induced acute lung injury, said Benjamin Singer, ’07 MD, ’10 GME, the Lawrence Hicks Professor of Pulmonary Medicine and senior author of the study.
“We’ve identified a cell type that potentially opens up a lot of avenues for therapy. In the mice that we’ve modeled in this paper, we show that proof of concept and also what the determinants of the cells’ stability are,” said Singer, who is also vice chair for research in the Department of Medicine and an associate professor of Biochemistry and Molecular Genetics.
Regulatory T-cells (Tregs) are a subset of CD4 T-cells which help regulate inflammation and promote the repair of damaged tissue, including the lungs following viral pneumonia-induced lung injury.
Previous work has shown that giving patients Tregs isolated from umbilical cord blood is a promising approach for promoting tissue repair following acute lung injury. Unfortunately, the number of circulating Tregs in the body is scarce, according to Singer.
“Only about five to 10 percent of your CD4 T-cells are regulatory T-cells, so getting enough of them to give to patients can be a problem,” Singer said.
In the current study, Singer’s team used an approach involving molecular stimulation and cytokines to turn conventional T-cells into induced Tregs (iTreg), which have similar cellular properties to naturally occurring Tregs.
The scientists then aimed to determine whether these iTregs could promote lung tissue recovery by transplanting the iTregs into mice with severe influenza pneumonia.
Using a combination of RNA-sequencing and analysis techniques, the scientists discovered that the iTregs promoted lung tissue recovery in the mice. They also found that iTregs require a specific epigenetic regulator — ubiquitin-like with PHD and RING finger domains 1 (UHRF1) — to maintain their overall stability and ability to reach the lung.
“These iTregs were able to promote recovery after severe influenza about as well as natural Tregs. That was a wonderful thing to see, because we can make these cells in great numbers much more easily than we can get natural Tregs from a host,” Singer said.
The study demonstrates how taking conventional T-cells from donors or patients and transforming them into Tregs in a laboratory could be an effective cellular therapy for patients with severe viral pneumonia and acute respiratory distress syndrome, according to Singer.
Singer said his team will continue to investigate the molecular factors that support the stability of iTregs, which can inform the development of additional therapeutic approaches.
“Once you have those T-cells in the lab and you’re turning them into iTregs, you can make other modifications. At the same time, we’re looking at ways that you can modify them to make them more stable and more effective so we can really make them the most effective therapy possible,” said Anthony Joudi, MD, a postdoctoral fellow in the Singer laboratory and lead author of the study.
Co-authors of the study include Jonathan Gurkan, a student in the Medical Scientist Training Program (MSTP); Elizabeth Steinert, PhD, research assistant professor of Medicine in the Division of Pulmonary and Critical Care; Manuel Torres Acosta, an MSTP student; Luisa Morales-Nebreda, MD, ‘17 GME, assistant professor of Medicine in the Division of Pulmonary and Critical Care; Carla Reyes Flores, a PhD student in the Driskill Graduate Program in Life Sciences (DGP); Hiam Abdala Valencia, PhD, associate professor of Medicine in the Division of Pulmonary and Critical Care; and Samuel Weinberg, ’19 MD, ’19 PhD, assistant professor of Pathology in the Division of Experimental Pathology.
Singer, Morales-Nebreda, Valencia and Weinberg are also members of the Center for Human Immunobiology.
This work was supported by National Institutes of Health grants F32HL162418, T32GM144295, T32HL076139, F31HL162490, T32AI083216, T32HL076139, T32HL076139, K08HL159356, U19AI135964, R01HL149883, R01HL153122, P01HL154998, P01AG049665, U19AI135964 and U19AI181102; the David W. Cugell Fellowship; Genomics Network (GeNe) Pilot Project Funding; the Parker B. Francis Opportunity Award; and the Burroughs Wellcome Fund Career Awards for Medical Scientists.