Fifty percent of men develop an inguinal hernia by age 75
By age 75, a noteworthy 50 percent of men develop an inguinal (groin) hernia — a bulge that results from soft tissue pushing through a weak spot in the abdominal muscles. Although common, the cause of these hernias is unknown, and the only treatment is surgery to repair the weakened area. Even after surgery, these hernias recur in 10 to 15 percent of men.
Using a novel, medication-based approach, a new Northwestern Medicine study published in The Journal of Clinical Investigation successfully reversed existing inguinal hernias in male mice and fully restored their normal anatomy without surgery. Even more promising, the scientists also examined human hernia tissue and found the identical molecular markers as in the mouse model. More than a million inguinal hernia repair surgeries per year are performed under general anesthesia in the U.S.
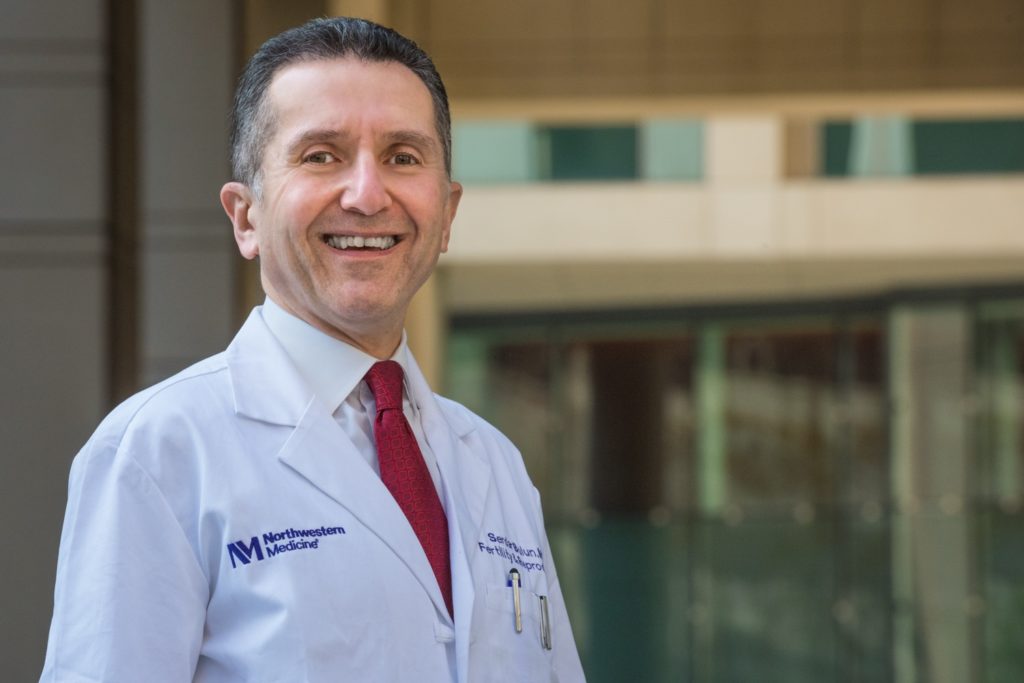
“This is a blockbuster publication about the first medical treatment of inguinal hernias,” said senior author Serdar Bulun, MD, the chair and John J. Sciarra Professor of Obstetrics and Gynecology and a Northwestern Medicine physician. “Our findings strongly suggest that men would also respond to this medication as the male mice did, so if male patients are high risk for surgery, we can one day try to repair the hernias medically.”
Lastly, the study found the likely cause of inguinal hernias: estrogen receptor-alpha (ESR1), which plays a key role in triggering the growth of certain connective tissue cells and the buildup of fibrous tissue, leading to the development of inguinal hernias.
How the study worked
The study was broken into two experiments: one using modified male mouse models and one examining human tissue.
In the mouse experiment, the scientists injected the anti-estrogen drug fulvestrant, which is currently approved to treat some types of breast cancer, into a humanized mouse model designed to mimic the higher estrogen levels found in aging men. When scientists blocked ESR1 in these connective tissue cells, it prevented muscle damage and hernia formation. Using fulvestrant in the study inhibited the ESR1 in the mice, which helped shrink large hernias and restore the mice back to their healthy anatomy.
In the human arm of the study, the scientists biopsied each participant twice — one from the hernia site and another from an adjacent healthy muscle — and found the same biological markers as in the mouse model. Further analysis showed that estrogen and ESR1 activate a set of genes linked to excessive tissue scarring, matching patterns seen in hernia tissue from human patients.
“We expect that estrogen/ESR1 is a promising molecular target for developing pharmaceutical treatments for inguinal hernia in men,” said corresponding author Hong Zhao, MD, PhD, research professor of Obstetrics and Gynecology in the Division of Reproductive Science in Medicine.
More about inguinal hernias
Inguinal hernias also occur in women but much less frequently (one woman for every 34 men). They recur in more than 10 percent of elderly male patients after an attempted surgical repair, which equates to roughly 100,000 elderly men a year, Bulun said. While these hernias are not typically painful, a patient can get very sick or even die if their bowel gets caught and becomes strangulated by the hernia.
Funding for the study was provided by the NIH grants R01-DK121529 and R01-DK139052.