For the first time, Northwestern Medicine scientists have identified a population of long-lived proteins in the ovaries which likely support the stability and longevity of the female reproductive system and may contribute to reproductive aging, according to a recent study published in the journal eLife.
“We’ve generated a resource for the field because now we have a catalog of long-lived proteins that we and others can now go after to understand mechanistically how they are contributing to reproductive aging,” said Francesca Duncan, PhD, the Thomas J. Watkins Memorial Professor of Reproductive Science, and co-senior author of the study.

As the body ages, all organ systems slowly decline in function. The female reproductive system, however, is one of the first organ systems to age, with fertility beginning to decrease in women in their mid-thirties and reproductive function stopping completely at menopause. Reproductive aging is also associated with a loss in egg quantity and quality, which can cause infertility, miscarriages and birth defects.
“The mammalian ovary is comprised of a fixed and nonrenewable pool of long-lived cells, or oocytes. They have to remain functional for up to decades in humans, so you can imagine that these cells are extremely vulnerable to any sort of damage that happens over that period of time,” said Duncan, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
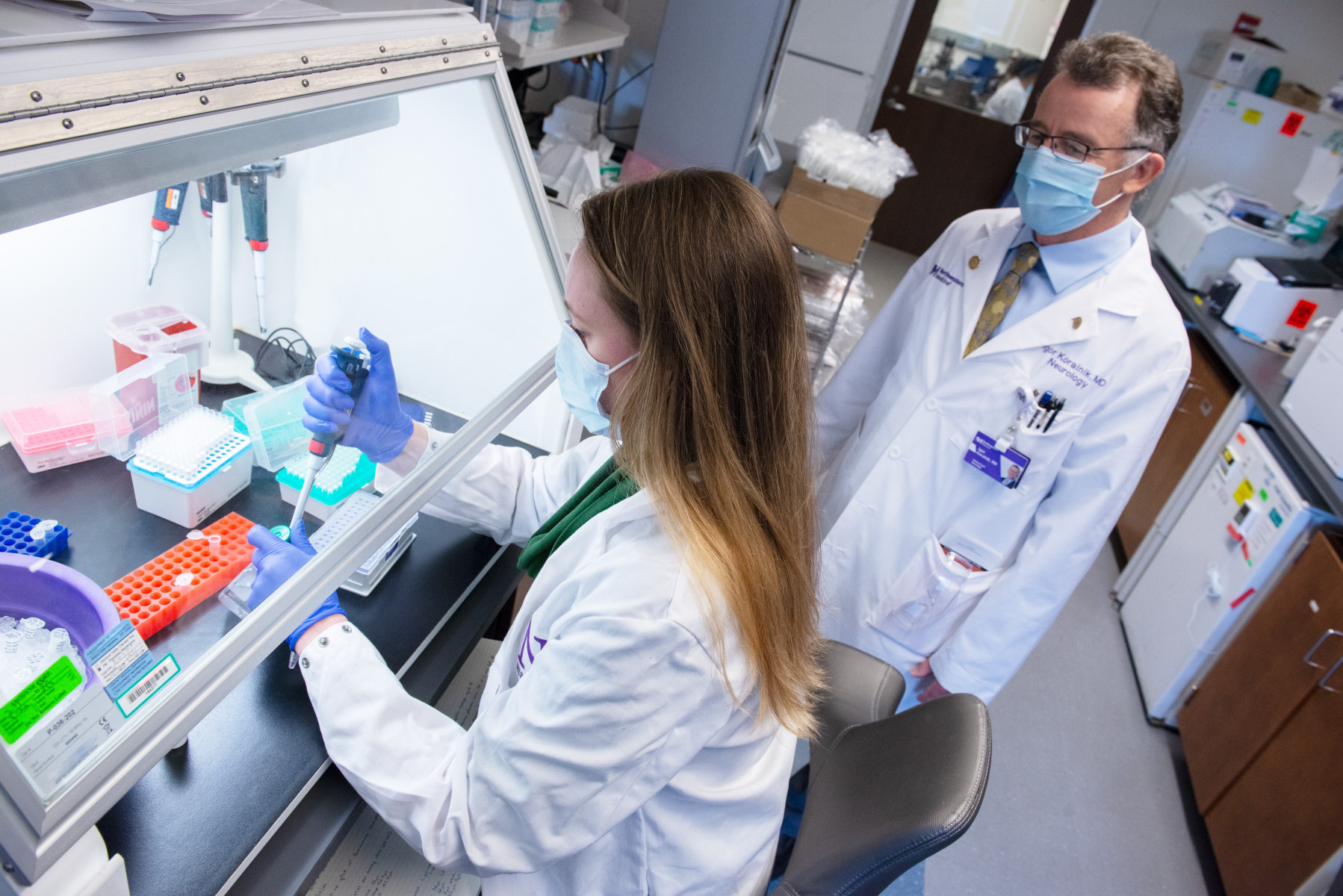
To better understand the mechanisms that contribute to reproductive aging, Duncan teamed up with Jeffrey Savas, PhD, associate professor in the Ken and Ruth Davee Department Neurology in the Division of Behavioral Neurology, to study the impact of the loss of protein function and quality in the ovaries and in oocytes, or egg cells that have not yet matured.
“You can imagine that if you have proteins in a cell that are sticking around for long periods of time without turning over, that could lead to damage in a long-lived cell,” Duncan said.
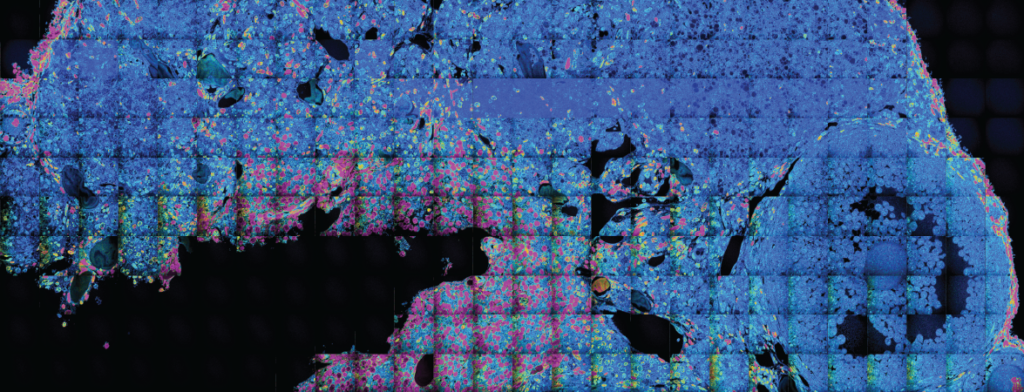
Using a comprehensive protein identification technique developed by Savas, which involved multi-generational whole animal metabolic stable isotope labeling and mass spectrometry-based quantitative proteomic approaches, the investigators were able to visualize and identify ovarian and oocyte long-lived molecules and proteins from mice at specific time points relevant to female reproductive aging.
“In the overall structure of the ovary, which contains oocytes and follicles, there’s a lot of diversity in terms of cell types and very specialized proteins are expressed there, so it seemed like a rich organ to study this aspect of biology,” said Savas, who is also a professor of Pharmacology and of Medicine in the Division of Nephrology and Hypertension.

In the mice oocytes and ovaries, the investigators found that long-lived proteins persisted after six months. At 10 months, however, most of these proteins had turned over and degraded. They also found increased subtypes of proteins in the oocytes, including histone proteins and several cytoskeletal proteins, as well as organ-specific proteins, including the ZP3 protein, which helps mediate sperm binding to the egg during fertilization.
Unexpectedly, the scientists also discovered a large percentage of these long-lived proteins were mitochondrial proteins; it is known that the mitochondria, the energy producing organelles of the cell, are essential for supporting egg quality. This may suggest that long-lived proteins are essential for ensuring the structural and functional integrity of oocytes, Duncan said.
“We know that with age, there’s deterioration of mitochondrial function, but long-lived proteins have never been implicated in the oocyte before, especially in terms of their mitochondria,” Duncan said. “This would suggest that the ‘scaffolding’ of the egg is actually made very early on and ultimately probably built upon with new proteins as the egg develops. This changes our fundamental understanding of egg biology and how we think about how these cells manage being long-lived.”
The findings underscore the role long-lived proteins have in maintenance and age-dependent deterioration of the female reproductive system.
The next steps in the investigation, according to Duncan, will be determining if these long-lived mitochondrial proteins are beneficial or damaging to oocytes over time and how this impacts overall egg quality and survival.
“I think this study is an excellent example of how at Northwestern interdisciplinary research can come together in highly impactful ways. It’s been incredibly exciting and rewarding to establish a common language and apply state-of-the-art technologies across disciplines to drive biology forward,” Duncan said.
Ewa Bomba-Warczak, PhD, a postdoctoral fellow in the Savas laboratory, and Karen Velez, MS, a former student in the Master of Science in Reproductive Science and Medicine program, were co-lead authors of the study.
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant R21HD098498), National Institute of Neurological Disorders and Stroke grants K99NS126639 and F32 NS106812, and National Institute on Aging grant R21AG072343.