Northwestern Medicine investigators have shed new light on how white blood cells in the retina function during inflammation and possibly during retinal vascular diseases with inflammatory components such as diabetic retinopathy, according to a study recently published in the Journal of Clinical Investigation.
Diabetic retinopathy – a complication of diabetes that can cause vision loss and blindness – affects an estimated 9.6 million people in the U.S., according to the Centers for Disease Control and Prevention.
While conducting prior research, Jeremy Lavine, MD, PhD, assistant professor of Ophthalmology and senior author of the study, noticed a buildup of white blood cells, particularly a subtype called macrophages, on the surface of retinas and along blood vessels in eyes affected by diabetic retinopathy.
In the current study, his laboratory set out to better understand and characterize these macrophages along blood vessels, and the roles they play in eye inflammation.
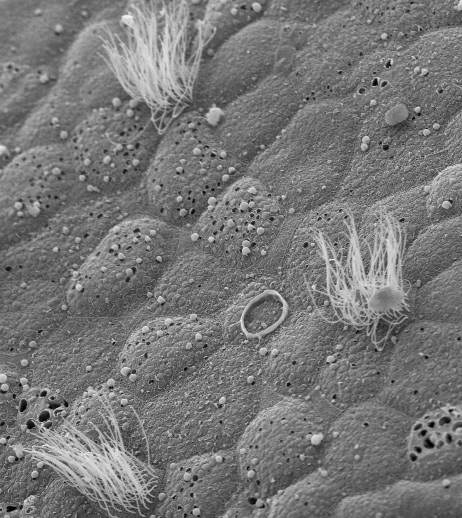
First, investigators utilized confocal immunofluorescence imaging to analyze mouse retina. They found that perivascular macrophages are distinct morphologically from microglia, and accumulate along venules, which are tiny blood vessels that branch off from veins.
“The location of these perivascular macrophages, uniquely along venules, makes them very interesting biologically because the pathophysiology of many retinal diseases results from excessive vascular leakage and immune cell extravasation, which both occur at venules,” said Lavine, who is also a professor of Medicine in the Division of Rheumatology.
Next, by employing single-cell RNA-sequencing, Lavine and his colleagues analyzed mouse retina affected by inflammation and found that retinal perivascular macrophages expressed higher levels of many chemokine genes like Ccl2 and Cxcl2.
Finally, in models of retinal inflammation, investigators observed that perivascular macrophage depletion led to a reduction in monocytes, another type of white blood cell that plays a key role in immune responses.
“The gene expression profile of perivascular macrophages shows an enrichment for chemokines, which bring in other immune cells. When we knocked out perivascular macrophages, we were able to reduce immune cell extravasation, suggesting that they’re participating in getting immune cells out of the vasculature and into the tissue in response to a stimulus,” Lavine, a member of the Center for Human Immunobiology, said.
Taken together, the findings of the study suggest that perivascular macrophages play a larger role than previously thought in eye disease, especially diseases involving inflammation or vascular leakage.
“In ophthalmology, any macrophage in the retina is a microglia – no one differentiates them,” said Lavine, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “One of the biggest takeaways of this study is that retinal perivascular macrophages are very different from microglia – and we’re still trying to learn in what other ways they’re different – but they have a very different transcriptional signature, express different markers and exist in different locations.”
Building upon his laboratory’s latest findings, Lavine will study the role of perivascular macrophages in uveitis, a rare eye condition that causes inflammation in the uvea, the middle layer of the eye’s pigmented tissue.
The study was supported by a grant from the nonprofit Research to Prevent Blindness, with additional funding from National Institutes of Health grants K08 EY030923, R01 EY034486 and the Research to Prevent Blindness Sybil B. Harrington Career Development Award for Macular Degeneration.