
Blocking the PD-1 inhibitory pathway within a subset of specialized T-cells may improve overall immune response against virally driven cancers, according to findings published in Nature.
Rebecca Obeng, MD, PhD, MPH, assistant professor of Pathology in the Division of Gastrointestinal and Hepatobiliary Pathology and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, was a co-author of the study.
T-cells, which contain receptors that allow them to recognize and attack foreign substances, differentiate into various cell subtypes, which help shape and control the immune response. One of those subtypes are cytotoxic CD8 T-cells, which directly kill virus-infected and cancerous cells. Proper activation and function of these cells is also critical for effective immunotherapy treatment for cancer patients.
Previous work had demonstrated that compromised CD8 T-cell function is caused by the increased expression of the inhibitory protein receptor molecule PD-1 on the cell surface. This leads to what scientists call “T-cell exhaustion,” in which CD8 T-cells ultimately lose their function over time.
Generally, this process helps the immune system resolve itself after it has been activated. However, in the case of chronic infection and cancer, PD-1 levels are consistently elevated which can prevent the proper functioning of CD8 T-cells and the immune response.
In the current study, investigators analyzed PD-1 positive CD8 T-cells from patients diagnosed with human papillomavirus (HPV)-positive head and neck cancer, which provided investigators the opportunity to examine tumor-associated virus-specific T-cells within a tumor’s microenvironment, according to Obeng.
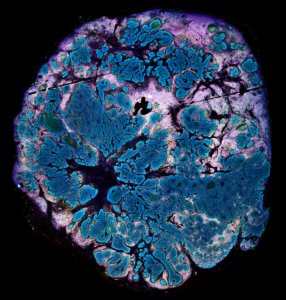
Using RNA sequencing, the team identified three subsets of PD-1 positive CD8 T-cells: One subset expressed the TCF7 gene and other genes associated with PD-1 positive CD8 T-cells that are essential for the survival of T cells; the second subset expressed more effector molecules, representing a transitory cell population; and the third subset was characterized by a terminally differentiated gene signature in which they are unable to differentiate into other cell types.
When the investigators treated the PD-1 positive CD8 T-cells with an HPV peptide and blocked the PD-1 cellular pathway, only the first subset of cells that express TCF7 proliferated and differentiated into effector CD8 T-cells. This subset is referred to as stem-like cells because they can regenerate and turn into other CD8 T-cell subsets, according to Obeng.
“The initial thought was that when you block the PD-1 pathway, you were reinvigorating the CD8 T-cells and recovering their function in some way. Now, we know that you may not only be reinvigorating the CD8 T-cells, but also driving the differentiation of new effector cells from these stem-like CD8 T-cells,” Obeng said.
The current findings suggest that additional antigen fragments from HPV proteins E2 and E5 identified by the investigators should be considered as targets for future vaccines. Furthermore, the findings underscore the importance of the tumor’s microenvironment and how therapeutic inventions can change a tumor’s microenvironment and impact the overall immune response, Obeng said.
This work was supported by the Ambrose Monell Foundation; the T. J. Martell Foundation; National Institutes of Health grants 5U19AI057266 and P01AI056299; the Oliver S. and Jennie R. Donaldson Charitable Trust; a Winship Invest$ Pilot grant; Swiss National Science Foundation grant P300PB_174483; a Eugenio Litta Foundation grant; NCI grant 1-R00-CA197891; the James M. Cox Foundation and James C. Kennedy; the Prostate Cancer Foundation; and a Triological Society Research Career Development Award.






