Whole-genome sequencing analysis of cutaneous T-cell lymphomas has revealed that deletions of the gene PD1 were associated with worse prognoses, according to a recent Northwestern Medicine study published in Blood.
Normally, PD1 codes for a receptor that acts as a check on T-cell activity to prevent over-activity and autoimmunity. Some immunotherapies suppress the PD1 receptor to unleash the body’s immune system against cancer, but this study demonstrates that cutaneous T-cell lymphomas (CTCLs) may be a poor candidate for this type of immunotherapy, according to Jaehyuk Choi, MD, PhD, the Ruth K. Freinkel, MD, Research Professor and senior author of the study.

“We’ve identified a cohort of patients that look the same as other patients molecularly, cellularly and have the same prognosis, but we think they should be treated differently,” said Choi, who is also an associate professor of Dermatology and of Biochemistry and Molecular Genetics.
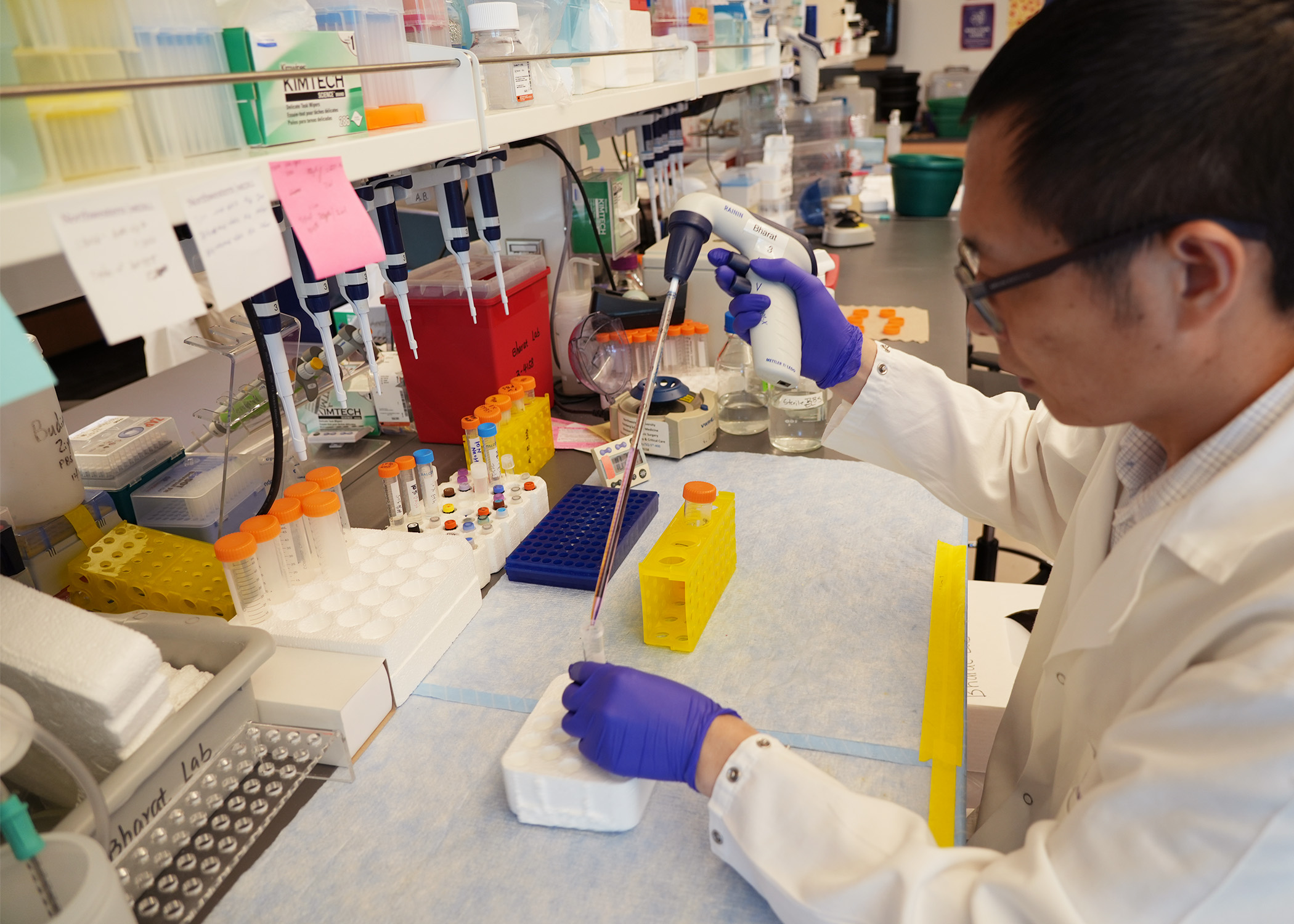
CTCLs are a clinically heterogeneous collection of cancers arising in T-cells in the skin. Previous genetic analyses have generally used older sequencing techniques and largely examined leukemic disease, one subtype of CTCL, limiting their application, according to Jay Daniels, a sixth-year student in the Medical Scientist Training Program (MSTP) and co-lead author of the study.
“Previous results have been biased towards those two types of studies, so we wanted to leverage whole-genome sequencing and include patients with many different types of disease,” Daniels said.
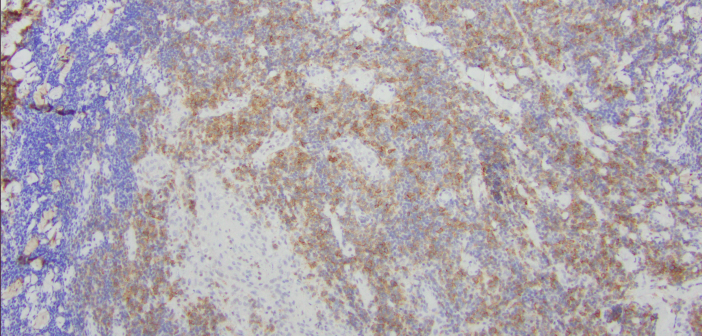
The study used more than 300 samples of CTCL from a diverse array of patients, including different subtypes, stages and outcomes. Using unbiased whole genome sequencing, the investigators found 86 putative driver genes and unexpectedly, one gene had a much stronger association with worse outcomes than the rest: PD1.
“We thought each gene would subtly be a driver of disease phenotype, so we were shocked when one gene seemed to explain the difference between very aggressive and less-aggressive cancer,” Choi said.
While the exact mechanism requires further study, Choi said this phenomenon made sense: In other cancers, suppressing PD1 helps recruit more T cells to fight cancer. But when the cancer arises from T-cells — as is the case in CTCL — shutting down a vital check on T-cell recruitment can fuel the cancer further.
These findings are concordant with previous research on PD1 immunotherapies and CTCL: While most patients do well on PD1 blockade immunotherapy, some patients get worse. Further, there are case reports of patients who received PD1 immunotherapy for different cancers and developed CTCL in the process.
“Those outcomes may have something to do with this mechanism,” Daniels said.
These findings indicate that clinicians need to be careful when using PD1 immunotherapy to treat patients with CTCL, and highlight the need for different immunotherapies for this subset of patients. This framework — more specific treatments, tailored to an individual’s genome — is a promising avenue for cancer therapy, Choi said.
“We have patients who have same diagnosis but very different clinical outcomes, so the ‘holy grail’ has been to figure out why these people are different,” Choi said. “If we know people have different biology, they’re going to respond to therapies differently, so that’s why we need to figure out what drives the heterogeneity from patient to patient.”
Choi is a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
This study was supported by National Institutes of Health grants K08-CA191019-01A1,1DP2AI136599-01, T32 CA009560, K08 AR072791 and P30 AR070253; the Skin Cancer Foundation, the Leukemia Research Foundation, the Doris Duke
Charitable Foundation, Damon Runyon Foundation grants DRCRF# CI-84-16, DDCF# 2016095 and DDCF CRM Award; and research grants from the Deutsche Forschungsgemeinschaft.