
Subcutaneous fat tissue expanded while insulin sensitivity improved after a gene transcription factor was deleted, according to a new Northwestern Medicine study published in Cell Reports.
This newfound function of the transcription factor, called BCL6, could have implications for obesity and Type 2 diabetes mellitus, according to Grant Barish, MD, assistant professor of Medicine in the Division of Endocrinology, Metabolism and Molecular Medicine and senior author of the study.
Previously, BCL6 had been studied extensively in the immune system, largely by scientists interested in B-cell and T-cell development, Barish said. However, recent work by the Barish laboratory revealed that BCL6 is also highly expressed in adipocytes, or fat cells.
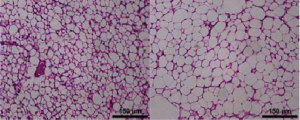
To investigate its function, Madhavi Senagolage, a seventh-year student in the Driskill Graduate Program in Life Sciences (DGP) and first author of the paper, deleted BCL6 from the fat cells of developing mice. Surprisingly, these mice selectively developed expanded subcutaneous fat tissue, but not intra-abdominal fat tissue — a rare example of a spontaneous phenotype impacting only certain body fat deposits.
“Most models of obesity have to be induced; you have to put them on a high-fat diet or give them a genetic background which causes them to eat excessively,” Senagolage said. “These mice eat the same amount, but they have all this fat just beneath the skin — that was very striking to us.”
Interestingly, deleting BCL6 in adult mice expands all types of fat tissue, but it’s not yet clear why developmental deletion has a depot-specific effect, Barish said.
[pullquote]“Understanding the basis for this is a fundamental area of interest in understanding the physiology of diabetes.”[/pullquote]
Later, genome-wide DNA binding and RNA analysis revealed that BCL6 works to repress genes involved in the synthesis of fatty acids and growth. Once BCL6 was deleted, the expression of those genes was increased, leading to the related changes of fat tissue expansion in mice. The same regulatory effects could be shared in humans, as well, according to the authors.
Cancer drugs in development are targeting BCL6, and this discovery indicates that such compounds may have important effects in non-cancerous tissues, according to Barish.
“It’s possible that these drugs to treat lymphoma may have metabolic effects,” Barish said. “Whether they are favorable in the setting of fat or in the setting of other cell types remains to be seen.”
In addition, while BCL6 deletion produced fatter mice, the animals developed improved insulin sensitivity — the opposite of what is typically observed with obesity.
“Normally, the more obese someone is, the more insulin resistant they become — that’s why we have such a scourge of diabetes that tracks with the weight epidemic,” Barish said. “In contrast, mice lacking BCL6 in their fat are the opposite. They are more obese, yet less prone to diabetes.”
Understanding the basis by which obesity can be rendered more metabolically healthy could point to new strategies to treat diabetes. This could also could help scientists understand a curious sub-population of patients who retain insulin sensitivity despite being obese. In fact, some patterns of genes regulated by BCL6 have also been identified in metabolically normal-obese humans, according to Barish.
“This is a very unusual combination of obesity and insulin sensitivity, making these mice a particularly interesting model,” Barish said. “Understanding the basis for this is a fundamental area of interest in understanding the physiology of diabetes.”
Other Northwestern co-authors include Barish laboratory members Krithika Ramachandran and Meredith Sommars, sixth-year students in the DGP; Christopher Futtner, research associate; and Amanda Allred and Yasuhiro Omura, research technologists. Center for Translational Imaging members Daniele Procissi, PhD, research associate professor of Radiology and Cynthia Yang, a computational imaging and data processing technician, were also co-authors.
This work was supported by the Howard Hughes Medical Institute and National Institutes of Health grants DK057978, HL105278, R01DK108987, P30DK020595, and K08HL092298.






