An age-related increase in estrogen may be the culprit behind inguinal hernias, a condition common among elderly men that often requires corrective surgery, according to a Northwestern Medicine study published in Proceedings of the National Academy of Sciences.
The study, led by Serdar Bulun, MD, chair and John J. Sciarra Professor of Obstetrics and Gynecology, found that the lower abdominal muscles of mouse models are particularly sensitive to estrogen, developing scar tissue in response to increases in estrogen levels that weakens the abdominal wall and eventually causes a hernia.
When the investigators reduced estrogen with a drug compound, it prevented the hernias, suggesting a therapy with preventive potential in humans.
“It may make sense to treat at-risk men with an aromatase inhibitor that could decrease estrogen and strengthen the muscle,” said Bulun, also a professor of Obstetrics and Gynecology in the Divisions of Reproductive Endocrinology and Infertility and Reproductive Science in Medicine.
Inguinal hernias occur when tissue, such as the intestines, protrudes through the inguinal canal, a weak spot near the groin in the human abdominal wall. These hernias are the most common reason men go undergo surgery; there are over 700,000 inguinal hernia repair surgeries performed each year in the United States, according to the FDA. While the chances of an inguinal hernia increase as men age, the root cause remains unknown.
One other consequence of aging in men is that a larger share of testosterone is converted to estrogen, by a hormone called aromatase. Humans use more estrogen than other animals; for example, mice produce testosterone in the testes and convert it to estrogen there, while humans create testosterone in the testes and then it is converted to estrogen locally in fat, muscle and other peripheral tissue.

Bulun, whose chief scientific interests include breast cancer and gynecology, was investigating the effects of high estrogen in female mice. One experiment involved boosting estrogen levels by incorporating the human aromatase gene into the mouse genome, creating mice who would convert testosterone into estrogen throughout the body. Originally, he wasn’t even interested in the male mice — until an animal keeper at Northwestern spotted large hernias developing in only the males.
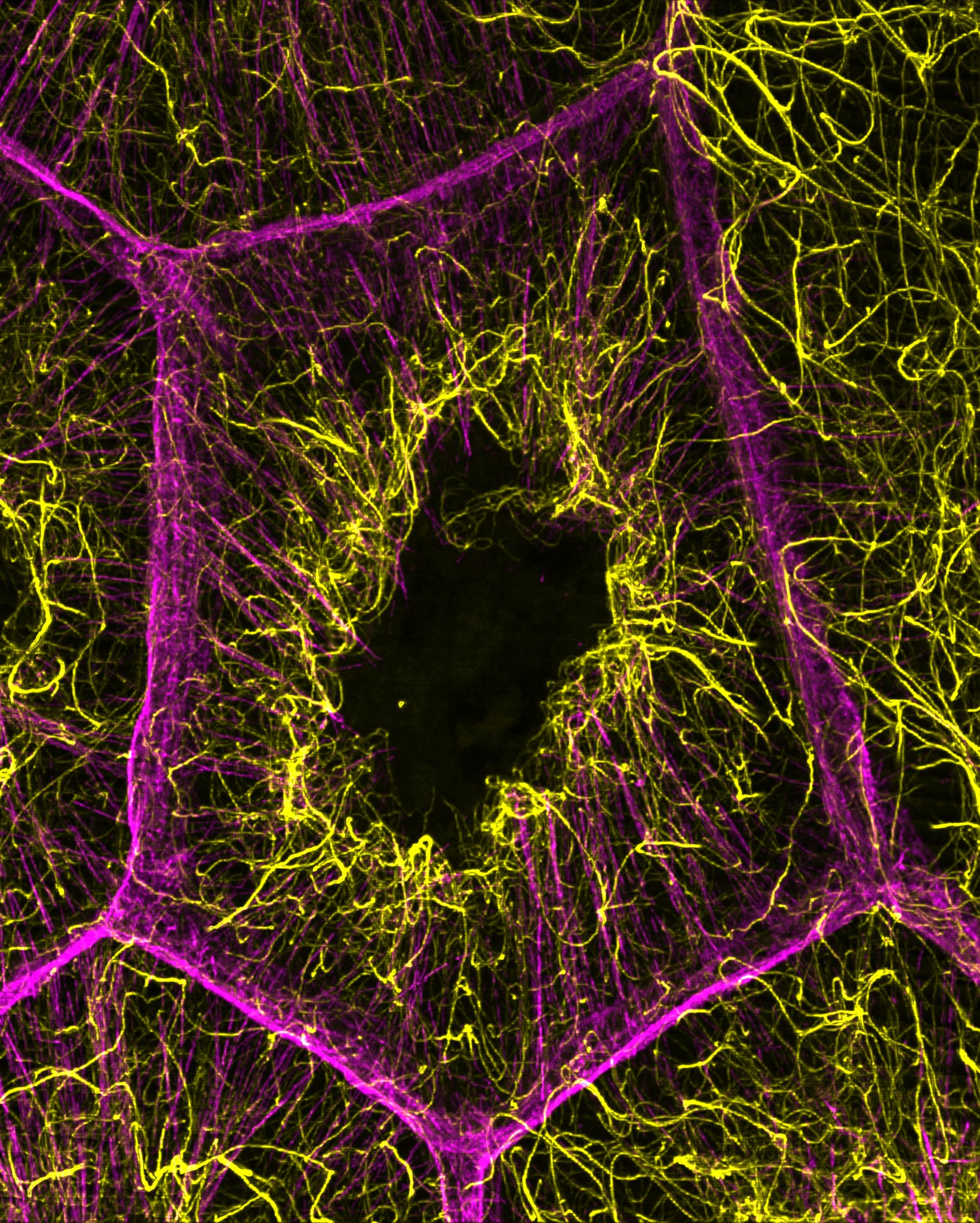
Bulun investigated these mice, finding large swaths of fibroblasts — scar tissue — developing in a small muscular sphincter, a structure analogous to the inguinal canal in humans.
“We realized the lower abdominal muscle is extraordinarily sensitive to estrogen,” Bulun said. “Estrogen causes these fibroblasts to divide rapidly, at a much higher pace than the muscle cells.”
The proliferation of the fibroblasts weakens the integrity of the sphincter and it eventually gives way, causing a hernia. When the investigators gave the mice a drug that blocked aromatase, and therefore the conversion of testosterone to estrogen, the hernias stopped, pointing towards estrogen as the cause — and according to Bulun, indicating potential for an aromatase inhibitor therapy that may be able to prevent surgery in at-risk patients.
Those patients with greater risk of hernia often have common factors like age or genetics, but overall, the best predictor of a future inguinal hernia is a past one, Bulun said.
“If you have to repair a hernia for the second time, the chances of success go down,” Bulun said. “If there is a recurrent case, you might be able to supplement the surgical treatment of that patient with medication.”
Bulun is currently working with Jonah Stulberg, MD, PhD, MPH, assistant professor of Surgery in the Division of Gastrointestinal Surgery and co-author of the current study, to design clinical trials that would test an aromatase inhibitor’s effectiveness in human subjects.
The first author of the paper was Hong Zhao, MD, PhD, research associate professor of Obstetrics and Gynecology in the Division of Reproductive Science in Medicine. Other Northwestern authors include Robert Chatterton, PhD, professor emeritus of Obstetrics and Gynecology in the Division of Reproductive Science in Medicine, and Warren Tourtellotte, MD, PhD, adjunct professor of Pathology.
This study was supported by National Institutes of Health grant R37-HD36891.
Bulun and Zhao are members of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.