In a large phase III clinical trial, a novel drug decreased mortality and hospitalizations of patients with transthyretin amyloid cardiomyopathy — a deadly heart disease with no current treatment.
The study, published in the New England Journal of Medicine, was co-authored by Sanjiv Shah, ’00 MD, professor of Medicine in the Division of Cardiology.
Shah was also the lead author of two recent studies, published in the European Heart Journal and JAMA Cardiology, that advance the understanding and treatment of heart failure with preserved ejection fraction (HFpEF), the most common form of heart failure.
All three studies were presented as late-breaking clinical trials at the European Society of Cardiology’s annual meeting, held in Munich August 25 to 29.
“The advances that we see here — one definitive therapy, another promising therapy and a deeper understanding of the underlying mechanisms of disease — demonstrate that we’re finally making headway in this clinical syndrome, and that Northwestern is leading the charge,” Shah said.
First Therapy for a Fatal Heart Disease
Cardiac amyloidosis is a rare and fatal condition where proteins abnormally build up within heart muscle, causing stiffening and eventually leading to heart failure.
One of the major subtypes of the disease is transthyretin cardiac amyloidosis, in which a protein called transthyretin becomes misfolded — either due to genetic inheritance or aging — and accumulates in the heart. There are currently no approved treatments for transthyretin cardiac amyloidosis, and average life expectancy after diagnosis is just three to five years.
Tafamidis is a novel oral medication that stabilizes the transthyretin protein, thus preventing it from unraveling and accumulating in heart tissue.
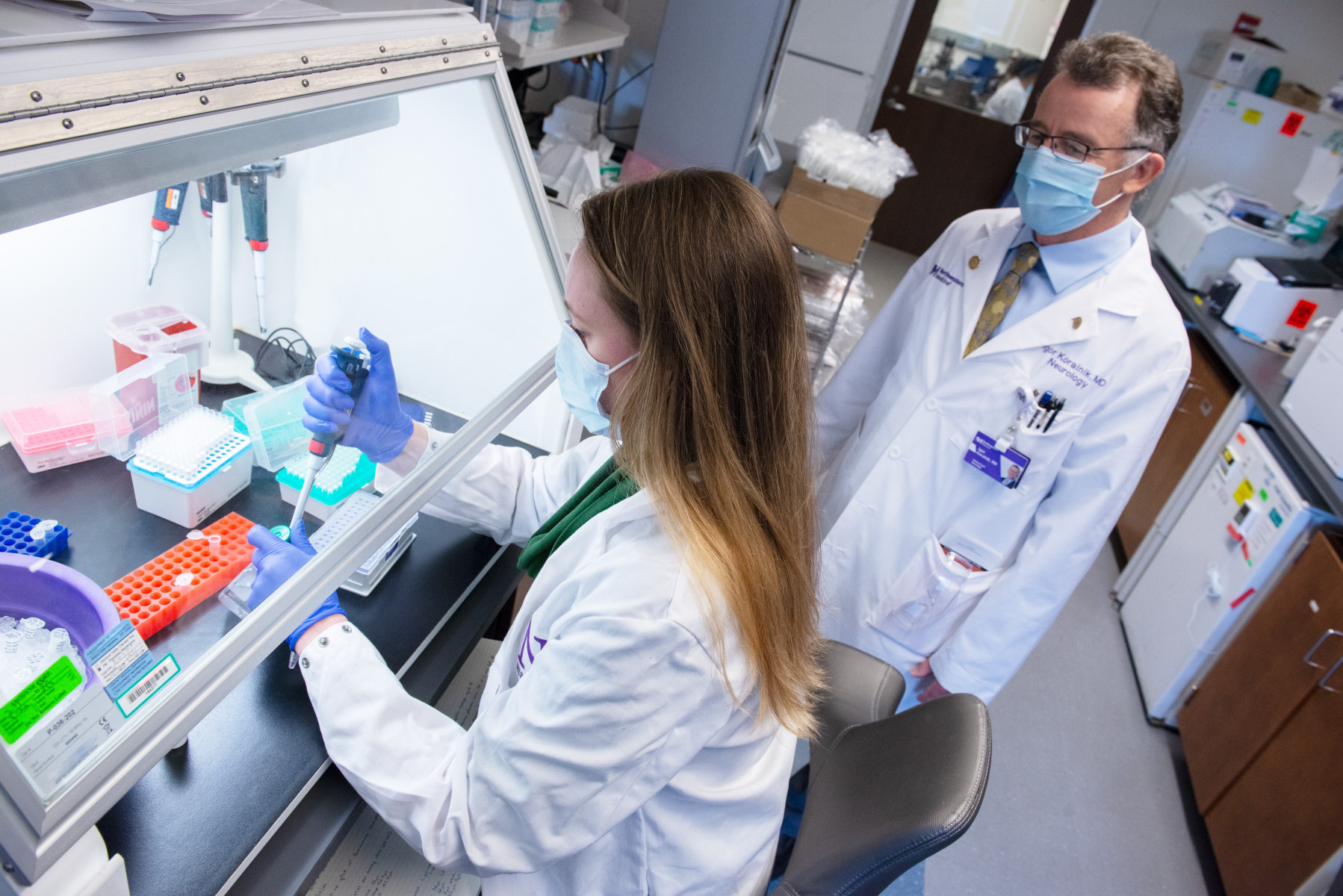
In a large, multisite phase III clinical trial, a team of investigators evaluated the efficacy and safety of tafamidis in patients with transthyretin cardiac amyloidosis. The trial, of which Northwestern was one of the top enrollers, randomized 441 participants to receive either tafamidis or a placebo.
The findings demonstrated that treatment with tafamidis reduced all-cause mortality and cardiovascular-related hospitalizations among study participants, compared to placebo. The drug also reduced the decline in both functional capacity — measured by distance walked over six minutes — and quality of life in patients.
“The results of the study are really remarkable,” Shah said. “Not only did the drug reduce mortality and hospitalizations, but people stayed healthier for longer, which we almost never see with a severe disease like this.”
Side effects were similar for participants in both the tafamidis and control group.
Tafamidis is currently in the process of FDA approval. Shah notes that investigations of other therapies for cardiac amyloidosis are also ongoing. “Our hope is that in the near future there will be multiple different treatments for this devasting disease,” Shah said.
The study was supported by Pfizer, which manufactures tafamidis.
Investigating Device for Heart Failure
About half of all heart failures cases are classified as heart failure with preserved ejection fraction (HFpEF), a condition where the heart is pumping normally but is abnormally stiff.
The syndrome is associated with significant morbidity and mortality, and is increasing in prevalence. There is currently no effective treatment.
In 2007, Shah established at Northwestern the world’s first specialized program dedicated to improving the prevention, diagnosis and treatment of HFpEF. The program investigates the disease in both laboratory models as well as population-based studies and large clinical trials.
One key feature of HFpEF is an increase in pressure in the left atrium during exercise. For close to a decade, Shah has been working with collaborators to develop a novel device to decompress the left atrium, which could improve both symptoms and outcomes in patients with HFpEF.
The Interatrial Shunt Device (IASD) is implanted into a patient’s interatrial septum, where it creates a small opening between the left and right atria. This opening is designed to allow blood to redistribute to the right side, reducing pressure in the left.
Shah is the principal investigator of a multicenter, phase II trial evaluating the use of IASD in patients with HFpEF. The trial includes 44 patients, half of whom were randomized to receive the device, with the other half receiving a sham procedure.
In a previous publication in Circulation, one-month findings from the trial demonstrated that the device reduced left atrial pressure during exercise and was safe, compared to the control group.
The current study, published in JAMA Cardiology, confirmed the safety of the IASD at the one-year mark.
“The trend is in the right direction — the device seems to be working in all patients, and to be safe — but it was a fairly small trial,” Shah explained. His team is now actively enrolling a large-scale randomized controlled trial to better determine the clinical efficacy of the IASD.
The study was also co-authored by Mark Ricciardi, MD, associate professor of Medicine in the Division of Cardiology, among others. Ted Feldman, MD, a cardiologist at NorthShore University Health-Evanston Hospital, was a co-principal investigator.
The study was funded by Corvia Medical Inc., which manufactures the device.
New Therapeutic Target for HFpEF
In the third publication, scientists also provided new insights into the pathophysiology of HFpEF.
It is the first prospective, multicenter study to demonstrate a high prevalence of coronary microvascular dysfunction — damage to the small blood vessels lining the inside of the heart — in HFpEF. The study, published in the European Heart Journal, could have important implications for the development of new therapies for HFpEF.
“We believe microvascular dysfunction is emerging to be central to the reason this kind of heart disease develops,” said Shah, who was the first author of the paper. “We’re now learning more about it from this study.”
The Northwestern HFpEF Program continues to be an active center in clinical trials for HFpEF treatments. Shah is also leading a number of new research projects in heart disease, including a National Institutes of Health-funded study to investigate using deep machine learning to diagnose cardiac amyloidosis earlier, among others.
The study in the European Heart Journal was supported by U.S. National Institutes of Health grants R01 HL105755 and R01 HL127028, American Heart Association grants #16SFRN28780016 and #15CVGPSD27260148 and a Clinician Scientist Award from the National Medical Research Council of Singapore.