A preliminary Northwestern Medicine study suggests that nonmyeloablative hematopoietic stem cell transplantation may reverse disability and improve quality of life for patients with relapsing-remitting multiple sclerosis (MS).
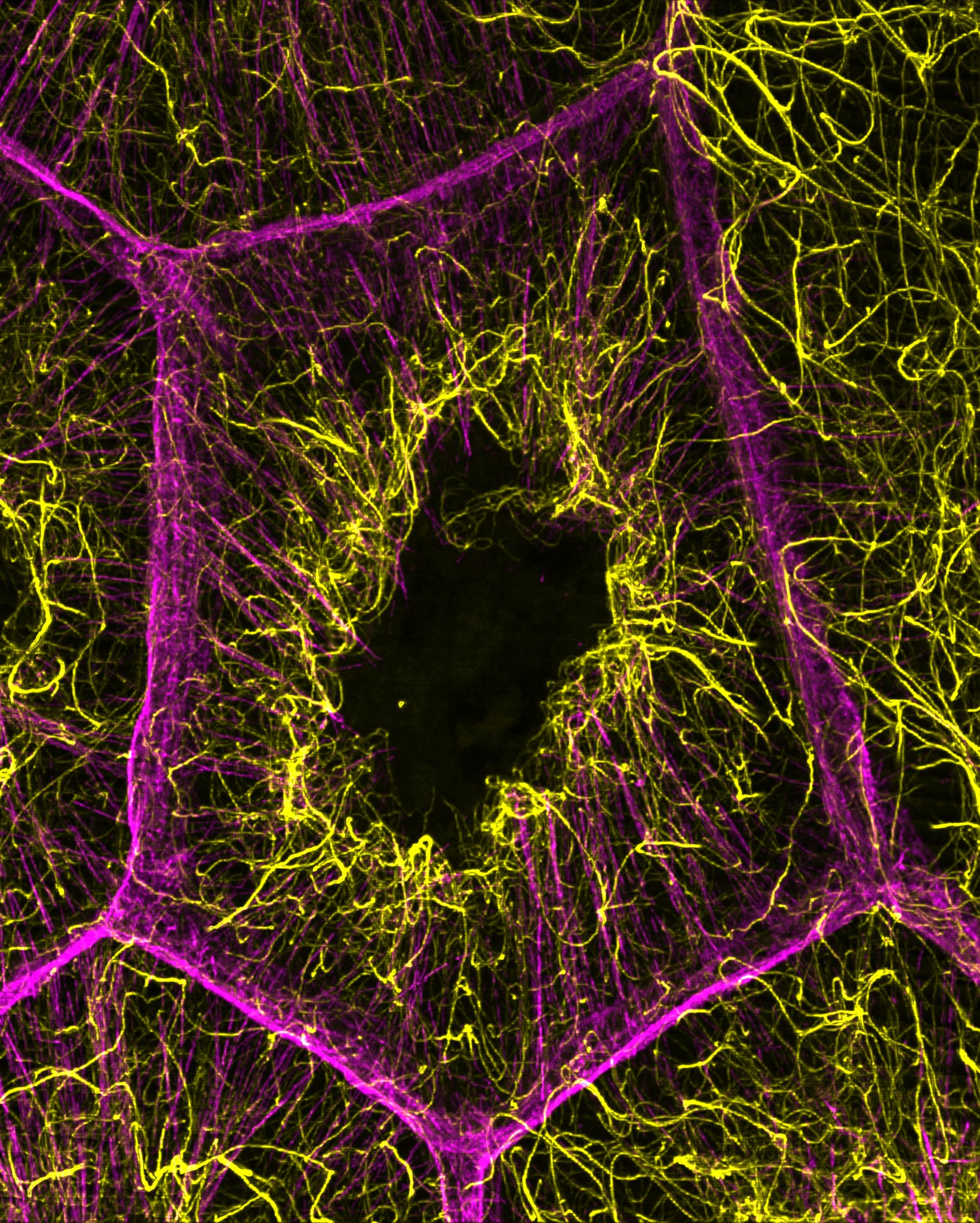
MS is an immune-mediated disorder of the central nervous system often arising in young adulthood. It damages the nerve cells in the brain and spinal cord, causing symptoms that range from fatigue to paralysis throughout life.
The study, published in JAMA, the Journal of the American Medical Association, included 145 patients with MS who underwent nonmyeloablative hematopoietic stem cell transplantation, a low-intensity stem cell therapy that uses a patient’s own blood-forming cells to reset the immune system.
“The drugs currently used to treat MS slow progression of disability,” said Richard Burt, MD, chief of Medicine-Immunotherapy and Autoimmune Diseases. “We show that one-time stem cell treatment can not only slow progression, but also reverse disability.”
Dr. Burt and colleagues examined the association between the stem cell transplantation and outcomes for patients with relapsing-remitting MS (the most common subtype of the disease, which is marked by periodic attacks followed by partial or complete recovery) and secondary-progressive MS (a more severe form of the disease without relapses, which follows relapsing-remitting MS).
Measuring disability on the Expanded Disability Status Scale, the study showed significant improvement for 50 percent of patients tested 2 years after treatment and for 64 percent of those tested after 4 years. There were also improvements in physical and cognitive function, quality of life scores and volume of brain lesions seen in MRI. These findings were seen only in patients with relapsing-remitting MS.
“These results are very promising and they could change the goal-line in this disease,” Dr. Burt said. “But a caveat is that you have to select the right group of patients.”
In addition, he notes that this study was observational, without a control group. An ongoing randomized trial with sites at Northwestern, Uppsala University in Sweden, the University of Sheffield in England and the University of Sao Paulo in Brazil, aims to confirm the findings.
Should the clinical trial be successful, investigators will next consider the long-term cost effectiveness of the stem cell therapy, said Dr. Burt. Previous studies have shown that the annual cost for treatment to slow MS progression is about $47,000 a year, and patients need to take current drug treatments for the rest of their lives.
“The stem cell therapy gets patients off lifelong treatments and gives them results that have never been seen before with this disease,” Dr. Burt said.
Additional Feinberg authors include Xiaoqiang Han, MD, Amy Morgan, NP, Kathleeen Quigley, RN, Kim Yaung, RN, Irene Helenowski, PhD, Borko Jovanovic, PhD, associate professor in Preventive Medicine-Biostatistics, Dzemila Spahovic, MD, Indira Arnautovic, MD, Daniel Lee, MD, ’02, ’06 GME, assistant professor in Medicine-Cardiology and Radiology, Brandon Benefield, and Stephen Futterer, MD, assistant professor in Radiology.
This study was supported by the Danhakl family, Cumming Foundation, Zakat Foundation, McNamara Purcell Foundation and Morgan Stanley and Company.