It’s what wasn’t missing that sparked the curiosity of Marco Martina, MD, PhD, associate professor in Physiology.
Working with a newly created preclinical mouse model of ataxia, a neurological disorder characterized by loss of balance and coordination, Dr. Martina wondered why the Purkinje neurons linked to the condition persisted well past the onset of disease.
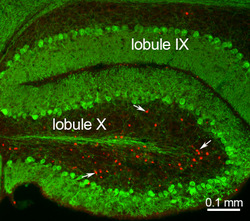
Closer inspection revealed that although the neurons had not died, they had been altered as early as a few weeks of age. It also uncovered that a different neuron population, unipolar brush cells (UBC), had been completely eliminated within a month of disease onset. Both changes were caused by the mutation of ion channel TRPC3, a known factor in the development of the disorder.
These findings were published in the Journal of Neuroscience.
“We are left with this double observation that even though the Purkinje neurons are still alive, they are functionally altered at a much earlier stage than previously thought, and the UBCs might play a role in development of ataxia,” said Dr. Martina. “What we do not know yet is whether the Purkinje neurons are causing all of these changes, or if the disappearance of UBCs are also contributing to the disorder.”
An estimated 150,000 Americans are affected by different forms of ataxia, which can strike at any time. Although the disorders are relatively rare, because they are neurological, Dr. Martina believes the findings in his lab could have much broader implications.
“A central question of cell biology and neurology, in terms of understanding the causes of all neurodegenerative disease, is what makes some cells more susceptible to cell death than others,” he said. “Here, we have a situation in which we know that a mutation of TRPC3 causes UBC death within 15 days, but that same mutation doesn’t impact Purkinje neurons for one month, and one year later has killed only 15 percent of the cells.”
By understanding more about cell death in ataxia, scientists may gain insight into the mechanisms that lead to selective vulnerability, an essential question in Parkinson’s, Huntington’s and Alzheimer’s disease.
The lab will next pursue the molecular pathways in Purkinje and unipolar brush cells that are activated after TRPC3.
“We also already have a molecule that blocks this TRPC3 channel and so will attempt to determine if it can prevent cell death,” Dr. Martina said. “If it works, an ideal future might include genetic screening of children for ataxia and exposure of the compound to at-risk populations.”
The work was supported by National Institutes of Health grant NS 09904.






