A Northwestern Medicine scientist has developed the first blood test to diagnose major depression in teens, a breakthrough approach that allows an objective diagnosis by measuring a specific set of genetic markers found in a patient’s blood.
The current method of diagnosing depression is subjective. It relies on the patient’s ability to recount his symptoms and the physician’s ability and training to interpret them.
Diagnosing teens is an urgent concern because they are highly vulnerable to depression and difficult to accurately diagnose due to normal mood changes during this age period.
The test also is the first to identify subtypes of depression. It distinguished between teens with major depression and those with major depression combined with anxiety disorder. This is the first evidence that it’s possible to diagnose subtypes of depression from blood, raising the hope for tailoring care to the different types.
“Right now depression is treated with a blunt instrument,” said Eva Redei, PhD, a professor of psychiatry and behavioral sciences at Northwestern University Feinberg School of Medicine and lead investigator of the study, published in Translational Psychiatry. “It’s like treating type 1 diabetes and type 2 diabetes exactly the same way. We need to do better for these kids.”
“This is the first significant step for us to understand which treatment will be most effective for an individual patient,” added Redei, also the David Lawrence Stein Professor of Psychiatric Diseases Affecting Children and Adolescents. “Without an objective diagnosis, it’s very difficult to make that assessment. The early diagnosis and specific classification of early major depression could lead to a larger repertoire of more effective treatments and enhanced individualized care.”
The estimated rates of major depressive disorder jump from 2 to 4 percent in pre-adolescent children to 10 to 20 percent by late adolescence. Early onset of major depression in teens has a poorer prognosis than when it starts in adulthood. Untreated teens with this disease experience increases in substance abuse, social maladjustment, physical illness and suicide. Their normal development is derailed, and the disease persists into adulthood.
The depressed teens in the study were patients of Kathleen Pajer, MD, a co-first author of the study, and her colleagues from the Research Institute of Nationwide Children’s Hospital in Columbus, Ohio. Pajer is now head of Dalhousie University’s Division of Child and Adolescent Psychiatry in Nova Scotia, Canada.
The study subjects included 14 adolescents with major depression who had not been clinically treated and 14 non-depressed adolescents, all between 15 to 19 years old. The depressed and control subjects were matched by sex and race.
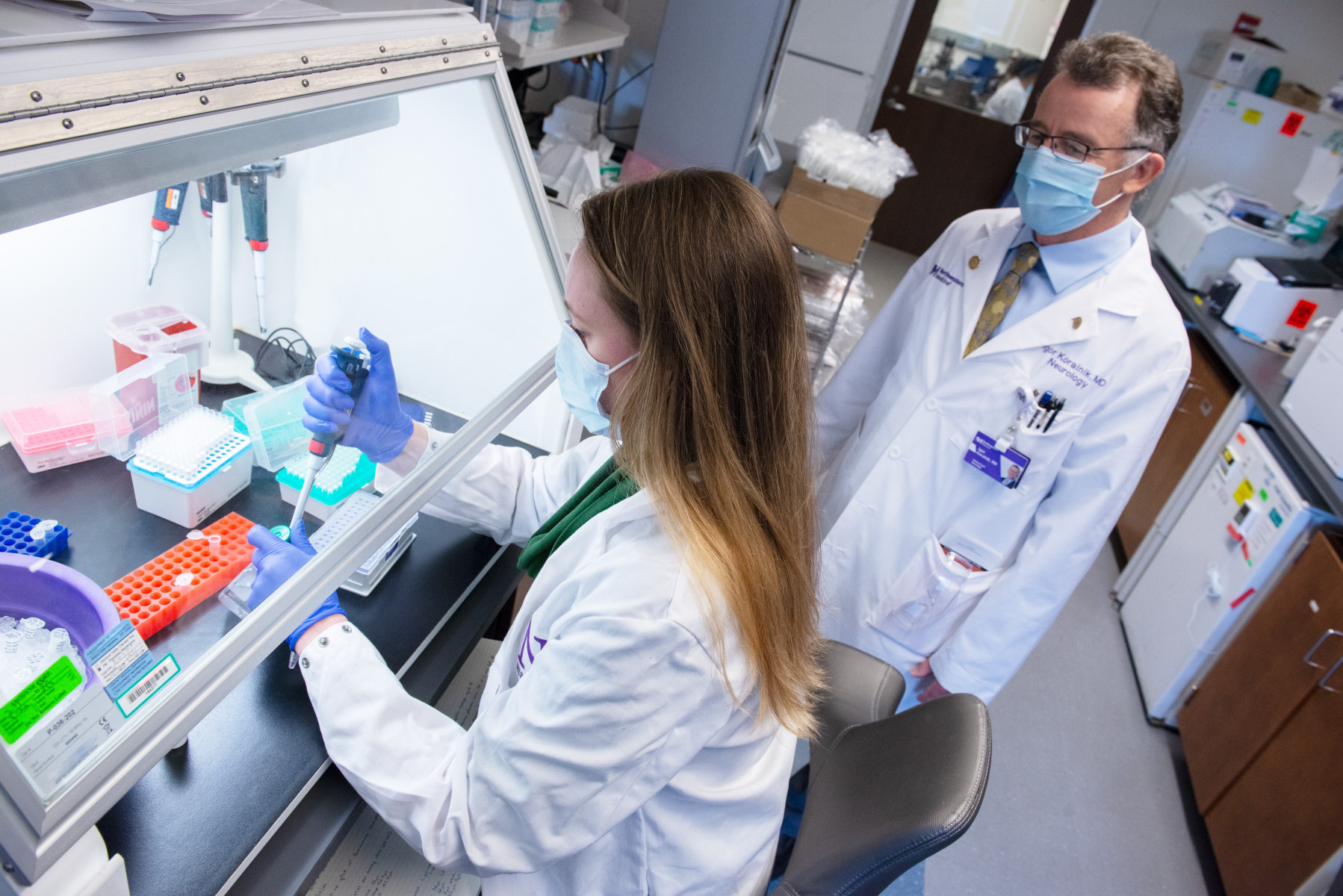
Redei’s lab tested the adolescents’ blood for 26 genetic blood markers she had identified in previous research. She discovered 11 of the markers were able to differentiate between depressed and non-depressed adolescents. In addition, 18 of the 26 markers distinguished between patients that had only major depression and those who had major depression combined with anxiety disorder.
The blood analysis was done by Brian Andrus from Redei’s lab, the other co-first author of the study, who was blind to the diagnoses of the subjects.
“These 11 genes are probably the tip of the iceberg because depression is a complex illness,” Redei said. “But it’s an entree into a much bigger phenomenon that has to be explored. It clearly indicates we can diagnose from blood and create a blood diagnosis test for depression.”
Redei first isolated and identified the genetic blood markers for depression and anxiety based on decades of research with severely depressed and anxious rats. The rats mirror many behavioral and physiological abnormalities found in patients with major depression and anxiety.
Further indicating the challenge in working with depressed adolescents, none of the teens who were diagnosed with depression opted for treatment.
“Everybody, including parents, are wary of treatment, and there remains a social stigma around depression, which in the peer-pressured world of teenagers is even more devastating,” Redei said. “Once you can objectively diagnose depression as you would hypertension or diabetes, the stigma will likely disappear.”
The human research was funded by grants from the Research Institute of Nationwide Children’s Hospital in Columbus, Ohio. Animal research was supported by grants from the Davee Foundation, the RD Foundation, and the National Institutes of Health.