Millions of “good” bacteria exist harmoniously on the skin and in the intestines of healthy people. When harmful bacteria attack, the immune system fights back by sending out white blood cells to destroy the disease-causing interlopers. But how do white blood cells know which bacteria are good and which are harmful?
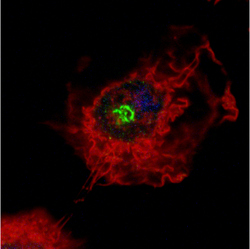
Northwestern University Feinberg School of Medicine researchers studied one type of white blood cell known as a macrophage, which is among the immune system’s first to detect and eliminate harmful bacteria. The research team, led by Christian Stehlik, PhD, John P. Gallagher Research Professor of Rheumatology at Feinberg, discovered that the protein NLRP7 serves as a “scout” in macrophage cells, identifying bacterial cell wall components in harmful gram-positive bacteria such as Staphylococcus aureus and Listeria monocytogenes. The findings were published in the February 23 issue of the journal Immunity.
“NLRP7 is a novel intracellular pattern recognition receptor that specifically recognizes bacterial cell wall components, known as lipopeptides, in harmful bacteria,” says Stehlik, who worked closely with collaborators Andrea Dorfleutner, PhD, research assistant professor of medicine at Feinberg, and Yon Rojanasakul, PhD, Robert C. Byrd Distinguished Professor and Benedum Distinguished Professor at West Virgina University. “We show that activation of NLRP7 is necessary for eradicating bacterial infections through the formation of protein complexes called inflammasomes, which enable the production of defense factors in immune cells.”
Identifying the molecule was complicated, says Sonal Khare, PhD, postdoctoral fellow at Feinberg and first author on the research paper, because the family of proteins within macrophages is quite large.
“There were 22 likely candidates. To determine which one of these proteins is able to recognize bacteria in macrophages, we had to remove each one of them,” she says. Through process of elimination, the team identified NLRP7 as the required protein.
Stehlik says the finding is significant because it contributes to a better understanding of how bacteria such as Listeria and Staphylococcus are recognized by the immune system. Listeria is found in uncooked meats, vegetables, and fruits such as cantaloupes. In 2011, Listeria was the cause of the deadliest food contamination outbreak in the U.S. in more than a decade. S. aureus infections are most commonly contracted in hospitals, and 500,000 patients acquire Staphylococcus infections annually in the U.S. Methicillin-resistant S. aureus, or MRSA, strains are highly resistant to commonly-used antibiotics. Understanding how the immune system recognizes these deadly intruders could one day lead to novel treatment strategies to combat these infections.
“The next phase of research related to NLRP7 and inflammasomes is progressing,” says Stehlik. “We are continuing the research to explore mechanisms behind how this NLRP7 inflammasome is formed. We want to know whether we can manipulate this process to make the response stronger. We also will be exploring the use of mouse models in this pathway to study this response in vivo.”
The article, “An NLRP7-Containing Inflammasome Mediates Recognition of Microbial Lipopeptides in Human Macrophages” will be available for download on the journal Immunity’s web site. This research was supported by grants from the National Institutes of Health, the American Heart Association, and the Arthritis Foundation.
To learn more about Stehlik’s research, visit his lab online.






