October 25, 2002
Smoking May Make Lymphoma More Lethal
CHICAGO— A Northwestern University investigator has hypothesized that smoking may play a dual role in the development of a cancer of the lymph glands called follicular lymphoma, first causing it to develop and then transforming it into diffuse large cell lymphoma, an aggressive cancer generally associated with a poor prognosis.
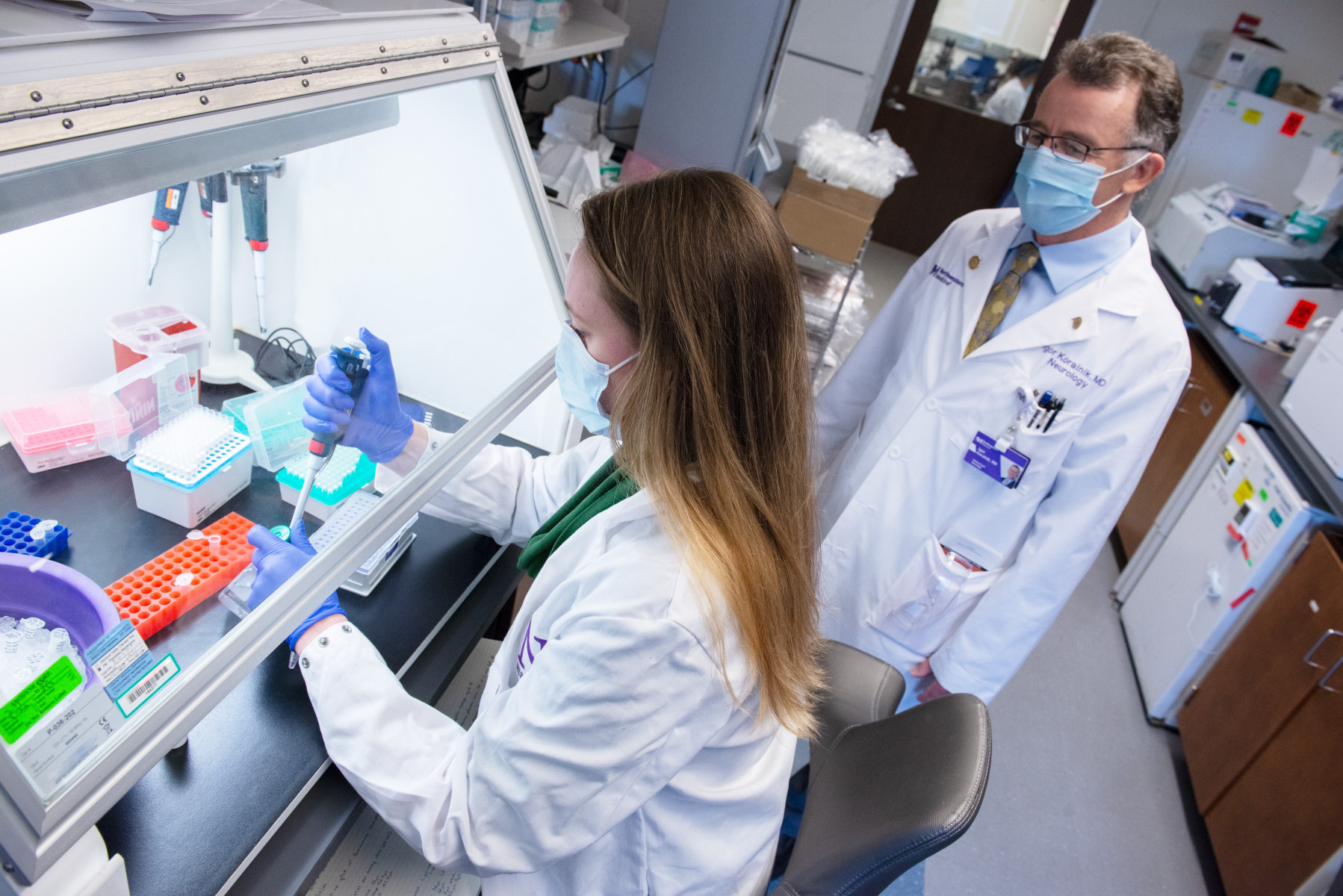
Cancer researcher Ronald B. Gartenhaus, MD, has been studying possible links between tobacco smoking and the genetic mutations associated with the transformation of follicular lymphoma, for which he recently received a $300,000 grant from the Flight Attendant Medical Research Institute. Dr. Gartenhaus is associate professor of medicine at The Feinberg School of Medicine and a researcher at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
More than 50,000 new cases of lymphoma were reported in 2001, a significant increase over the past 20 years even when HIV-related lymphomas are excluded. A small portion of the increased incidence of lymphomas has been attributed to exposure to chemical carcinogens such as herbicides and pesticides as well as to radiation. Now, smoking—long known to cause cancer of the lung and other organs—has been implicated in the development of a hematologic malignancy.
While this subset of lymphomas usually follows an indolent clinical course, a significant percentage transform into an aggressive large cell lymphoma with poor prognosis, Dr. Gartenhaus said. The vast majority of cases of follicular lymphoma have rearrangement of the Bcl-2 oncogene. The cases of follicular lymphoma that transform into diffuse large cell lymphoma have additional genetic alterations, particularly, mutations of the p53 tumor suppressor gene.
Research by others has shown that exposure to the aromatic hydrocarbons found in tobacco smoke causes distinct mutations in the p53 tumor suppressor gene. One of p53’s major roles is to arrest cells that have sustained DNA damage from proceeding into the phase of the cell cycle involving DNA synthesis.
If, however, the p53 gene is mutated and the cell divides before repair can occur, the errant DNA sequence is copied in its mutated form and daughter cells then inherit a mutated gene, which may confer a growth advantage or drug-resistant phenotype, Dr. Gartenhaus said.
He further noted that in some cases of transformed follicular lymphoma, a defect called microsatellite instability may occur, causing uncontrolled variation and “slippage” of coding sequences during DNA replication. A study performed elsewhere recently implicated smoking in the development of microsatellite instability in some forms of colon cancer.
Dr. Gartenhaus and his laboratory group are reviewing smoking histories of patients with transformed follicular lymphomas and examining tumor DNA to derive information about the frequency and spectrum of p53 mutations present in smokers and nonsmokers. They also are studying transformed lymphomas from both smokers and nonsmokers for the presence of microsatellite instability.
“If indeed smoking is associated with the development of microsatellite instability, the loss of DNA replication repair function may lead to increased mutations in genes critical to cell growth regulation and possibly drug resistance,” he said.
“The findings of our study may have therapeutic implications perhaps requiring alternative therapies in patients with these molecular defects,” Dr. Gartenhaus said.