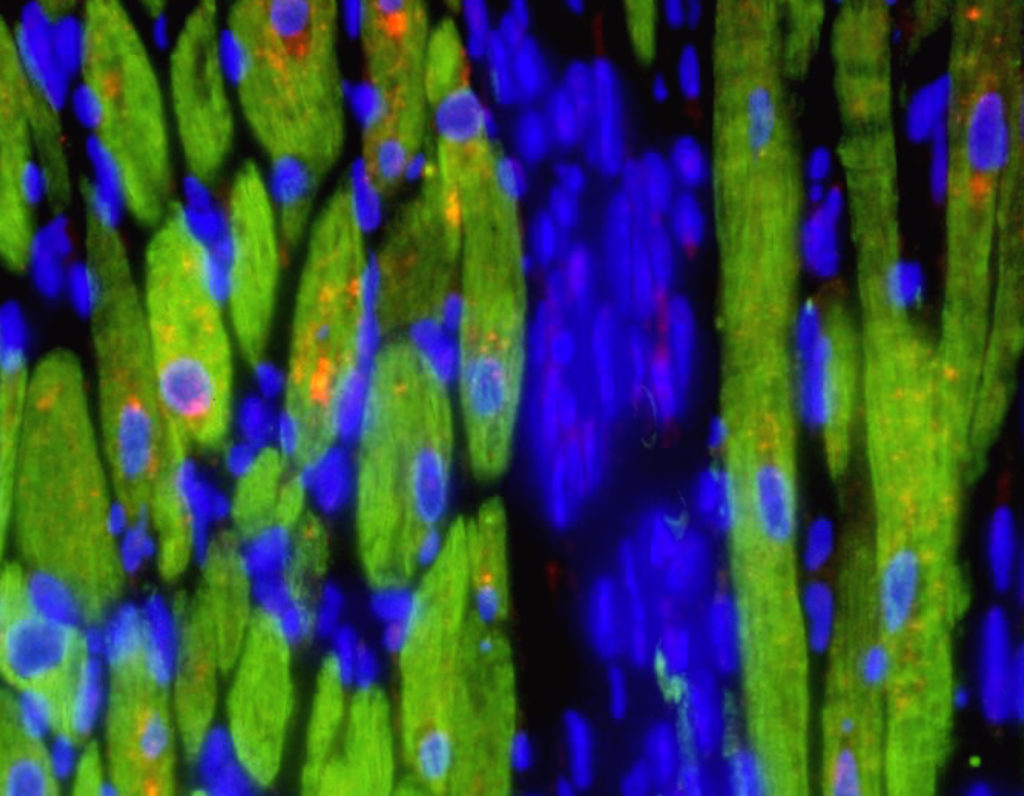
Northwestern Medicine scientists have identified a novel molecular mechanism that regulates scar formation in the heart, a common manifestation of aging and nearly every form of heart disease. The discovery was published in the journal Circulation.
The scientists showed that heart muscle cells called cardiomyocytes are a principal source of the molecular signals that drive scarring in the heart, a process known as cardiac fibrosis.
“Historically, these signals were thought to arise from other cell types in the heart,” explained Panagiotis (Peter) Flevaris, MD, PhD, ’12, ’17 GME, instructor of Medicine in the Division of Cardiology and first author of the paper. “We also identified the gene that serves as the master regulator of the synthesis and release of pro-fibrotic signals from heart muscle cells across different species.”
First, Flevaris and colleagues showed that a familial mutation in that gene, which encodes the protein plasminogen activator inhibitor-1 (PAI-1), leads to spontaneous cardiac fibrosis in otherwise healthy individuals in an Old Order Amish community. The findings in the human population confirmed previous observations in mice lacking the gene for PAI-1.
Importantly, the scientists found that a protein called bone morphogenetic protein 7 (BMP7) can prevent the generation of fibrotic signals by cardiomyocytes and may be able to serve as a future therapy for cardiac fibrosis.
“Tissue fibrosis is the leading cause of organ failure, but persists as one of the most pressing global health problems due to lack of effective pharmacotherapies. Currently, the only cure for cardiac fibrosis is heart transplantation,” said Flevaris, who completed this research during a post-doctoral fellowship in the Department of Medicine’s Physician-Scientist Training Program, working with senior author Douglas Vaughan, MD, Irving S. Cutter Professor of Medicine and chair of Medicine.
“Supported by clinical and functional data, our work provides exciting new evidence that modulation of cardiomyocyte signals by BMP7 represents a unique therapeutic strategy to prevent cardiac fibrosis,” Flevaris added. “This discovery not only provides a novel paradigm for how the heart muscle generates signals following injury, but also has the potential to transform healthcare for the heart failure population at large.”
This research was supported by National Institutes of Health grants R01 HL051387, F32 HL131301-01, and F32 HL129695-01, and American Heart Association grant 16GRNT31130010.






