In an effort to increase understanding of uterine fibroid development and growth, Serdar Bulun, MD, chair of obstetrics and gynecology at Northwestern University Feinberg School of Medicine, has authored a review article published in the October 2 issue of the New England Journal of Medicine that merges recent research about the disease. The piece pinpoints three elements that result in the most common tumor found in women.
“We have learned a lot about uterine fibroids over the past five years and there have been various high impact journal publications that have changed the focus of the field,” said Bulun, a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “Because each individual finding brought with it one piece of the puzzle, this article aims to bring them together under one unified hypothesis, providing a useful framework for scientists, clinicians, patients, and the pharmaceutical industry.”
In 2009, Bulun and colleagues Julie Kim, Debabrata Chakravarti, Erica Marsh, Takeshi Kurita, and JianJun Wei from Feinberg, and Romana Nowak from the University of Illinois at Urbana-Champaign, received a P01 grant to fund the only National Institutes of Health-supported comprehensive uterine fibroid research center in the country.
In June 2010, scientists at Feinberg, led by Kurita, redefined the roles that estrogen and progesterone play in the disease, a discovery that set the stage for major findings to come. That paper, published in Endocrinology, provided proof that estrogen promotes but does not cause uterine fibroid formation. The sex steroid works to prepare uterine tissue to respond to progesterone and to progesterone receptors, and it is these hormones that promote tumor growth.
“By identifying a plausible mechanism of tumor growth, it triggered the field to develop a drug that has already been approved in the European Union and Canada,” Bulun said. “Two papers published in 2012 in the New England Journal verified the role of progesterone and demonstrated the efficacy of an anti-progesterone drug to treat fibroids.”
If introduced in the United States in the near future, as Bulun suspects, it will mark the first time since the early ’90s that a new drug will be offered to fight uterine fibroids.

Stem Cells Carrying Mutations
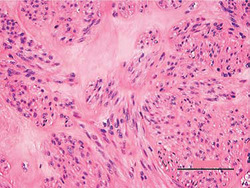
Although the cellular origin of fibroids remains unknown, several observations support the notion that each tumor originates from the transformation of a single somatic, or adult, stem cell.
In a 2011 paper published in Science, a single gene defect was found in a majority of uterine fibroids. A second project determined that the gene affected was MED12. Although not well understood, the gene is mutated in 80 percent of all fibroids.
The following year, Bulun’s lab published an article in PLOS ONE showing that the growth of fibroid tumors, dependent on estrogen and progesterone, also require the presence of these stem cells, which make up just one percent of the tumor. Most importantly, Bulun’s group reported that fibroid stem cells, but not the stem cells from the surrounding uterine tissue, carried MED12 mutations.
“It’s been really interesting how these three discoveries have changed the field. We’ve found out that if you don’t have the sex steroids, especially progesterone, if you don’t have the stem cells in the environment, and if these stem cells do not carry mutations, the most common of which is MED12, then you don’t have a tumor,” Bulun said.
Having pinpointed these crucial elements, Bulun believes scientists will now seek to develop new treatment strategies that target the small stem cell populations.
“It is a really exciting time,” Bulun said, “As we learn more about fibroids in the lab, we can follow the trail to further develop new treatments.”
Bulun’s research is supported by grant HD0577877, a five year P01 Program Project funded by the Eunice Kennedy Shriver National Institutes of Child Health and Human Development.






