The imbalanced activation of neural cells and previously unknown connections within the brain’s external globus pallidus (GPe) and striatum may be responsible for some motor symptoms in Parkinson’s disease and similar neurodegenerative conditions, according to a pair of Northwestern Medicine studies published in The Journal of Neuroscience.
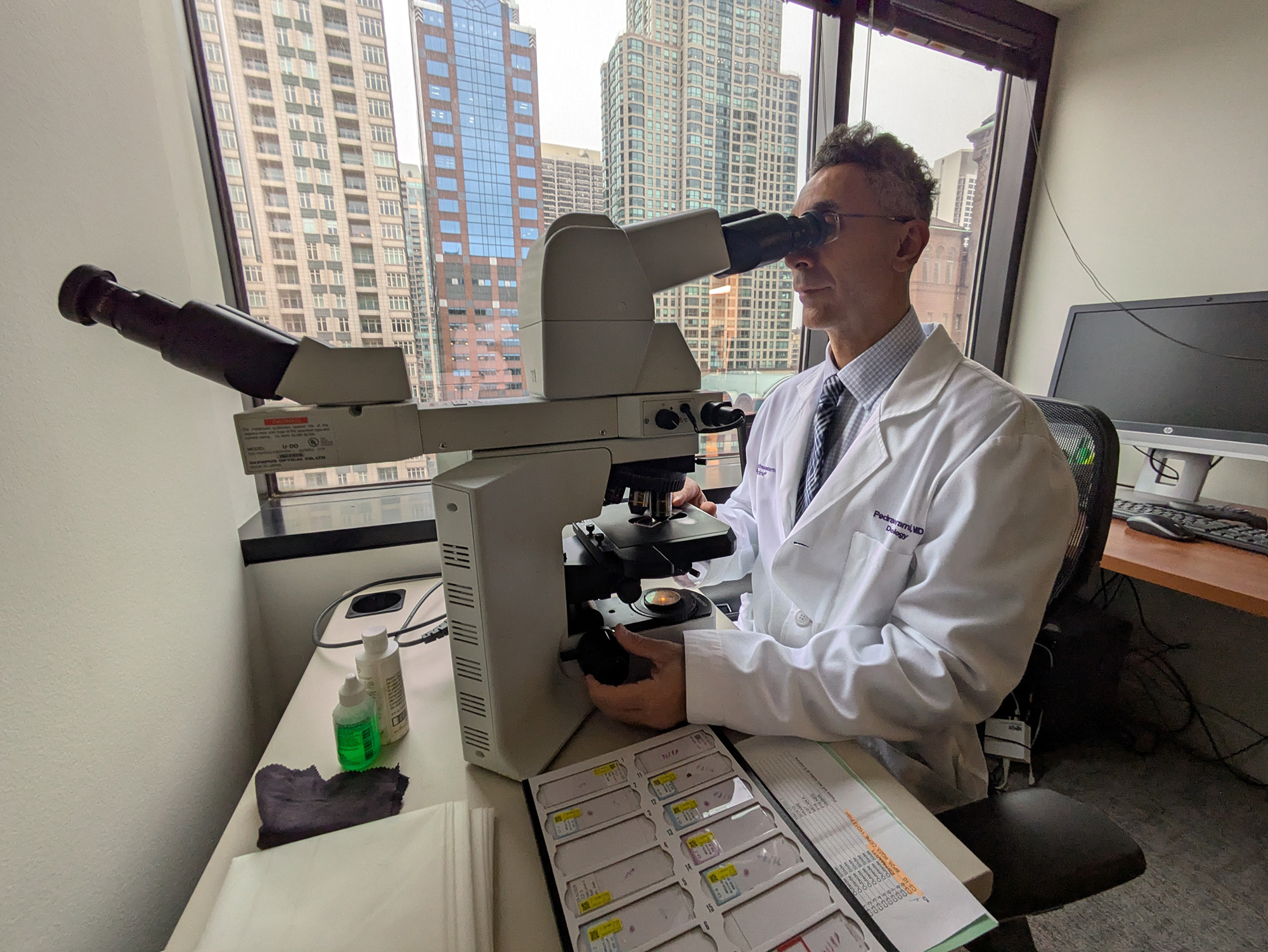
A more detailed neural map of these regions, plotted by Savio Chan, PhD, associate professor of Physiology and senior author of the studies, could help guide future attempts to manipulate these circuits in an effort to alleviate neurodegenerative diseases.
“Understanding how these circuits are altered could help us in the future to identify ways to fix the circuits when they go awry in disease conditions,” Chan said.
Neuronal Demographics
The GPe, part of the basal ganglia located at the base of the brain, is one half of the globus pallidus structure. The GPe is a major regulator of voluntary movement. However, until recently the GPe was mostly disregarded, according to Chan.
“It was a black box in this circuit — no one knew what it did, so it was overlooked and people didn’t pay attention to it,” Chan said.
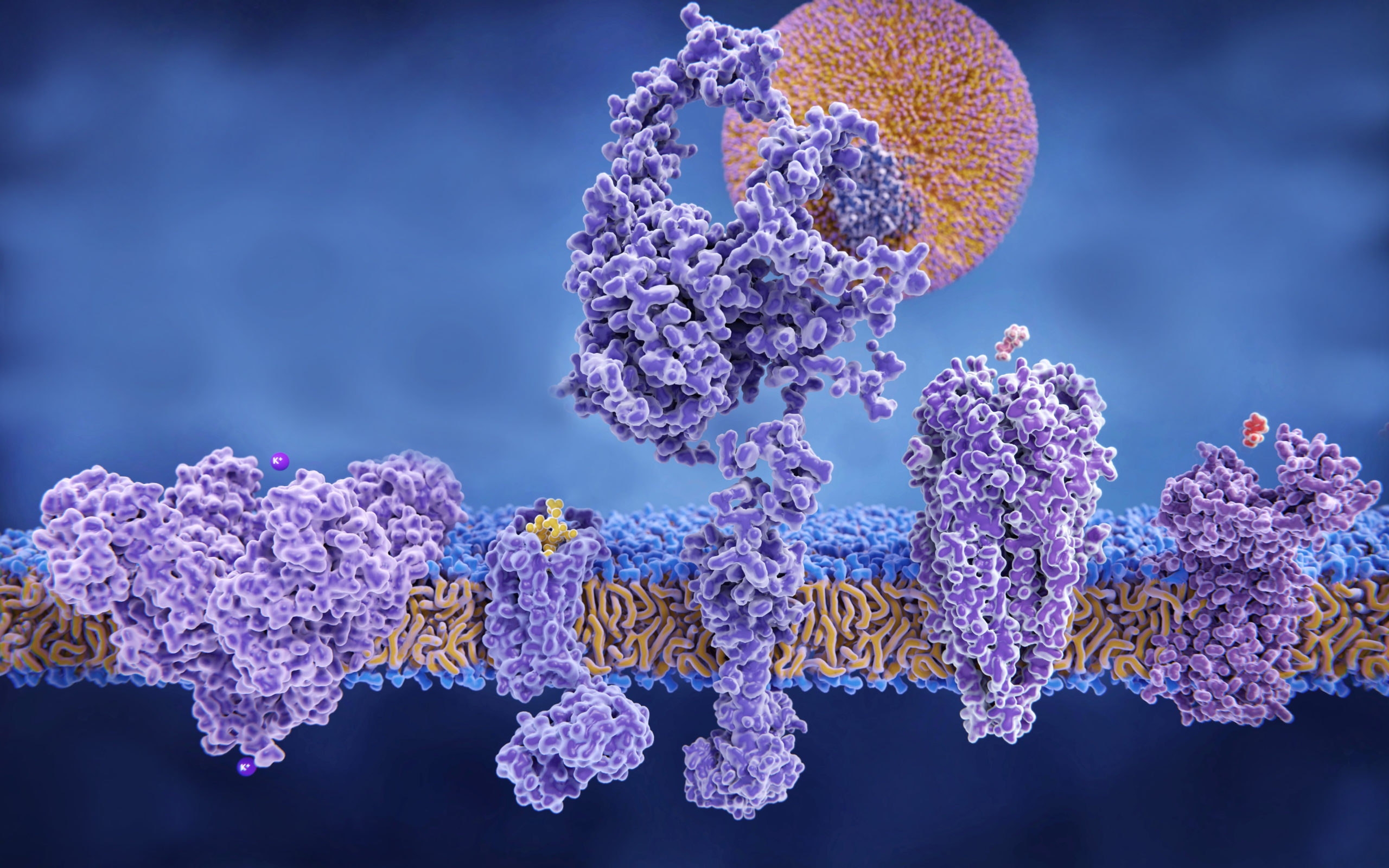
The GPe is largely made up of two classes of cells: Npas1 cells and PV cells, which suppress and promote motor system activation, respectively. In the study, Chan and his collaborators investigated the subtypes of these cell classes, discovering that several Npas1 subtypes project to different areas of the brain, including the striatum, the thalamus and the cortex.
In healthy subjects, the GPe exhibits what is called an activity-independent model: Neuron activity is unsynchronized, essentially a low constant hum of random activation. However, in the brains of patients with Parkinson’s disease, GPe neurons exhibit synchronous burst activity that correlates with motor symptoms.
Just by activating one subtype of Npas1 cells — called Foxp2 cells — the investigators were able to recreate gait freezing, a cardinal symptom seen in patients with Parkinson’s disease.
“It’s telling us that we don’t need the entire population of cells to be doing the same thing to see the motor outcome,” Chan said. “It’s possible that in Parkinson’s, these cells are overactive, which is something we want to explore.”
Plotting Unknown Pathways
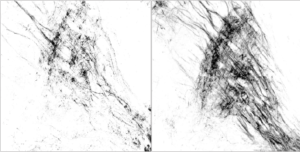
The striatum, located in the forebrain, is the largest input station of the basal ganglia, with two main output pathways characterized by their neurons: a direct pathway of spiny projection neurons (dSPNs) and an indirect pathway of spiny projection neurons (iSPNs).
It is generally assumed that the direct pathway promotes motor activity while the indirect pathway suppresses motor activity, at least from the dorsal medial striatum. While there are also connections running from the dorsal lateral striatum, these hadn’t been closely examined until now, according to Chan.
“People just assumed the lateral side would act exactly like the medial side,” Chan said. “Part of this was a lack of tools, but now with optogenetics, we can really tickle the circuit and see how it responds.”
In the study, Chan examined the function of these pathways, finding that the dorsal lateral striatum actually operated in the reverse; dSPNs caused motor suppression while iSPNs caused motor promotion.
“This was a complete surprise to us,” Chan said.
Further, when the investigators measured striatum input into the basal ganglia’s GPe specifically, they found a previously unknown role for dSPNs. While they provide only fraction of the input when compared to iSPNs, they were still a prominent regulator of motor activity, potentially through selectively targeting of Npas1 cells, Chan said.
Using mouse models of Parkinson’s disease, the scientists observed that dSPN projection to the GPe from the dorsal lateral striatum was dramatically strengthened, throwing the system out of balance and contributing to motor suppression symptoms in patients with Parkinson’s disease.
“Patients are moving very slowly or not very much at all, and this is a possible explanation,” Chan said. “This is a pathway that people had not thought mediated motor suppression.”
The discovery of this neural pathway opens the door to exploiting this population of dSPNs in a bid to reduce motor symptoms in patients with Parkinson’s disease, according to Chan.
“Once we make sense of how these circuits contribute to motor patterns, we can try to manipulate these circuits in disease conditions,” Chan said.
Qiaoling Cui, PhD, research assistant professor of Physiology, was lead author of both studies.
Both studies were supported by National Institutes of Health grants R01 NS06977734, R01 MH112768, R01 NS097901, R01 MH109466, R01 NS088528, T32 AG020506, T32 NS041234, F32 NS098793, R01 MH112768, R35 NS097185, a HHMI-PF Medical Research Fellowship and AΩA Student Research Fellowship.