Scan beats genetics to gauge risk
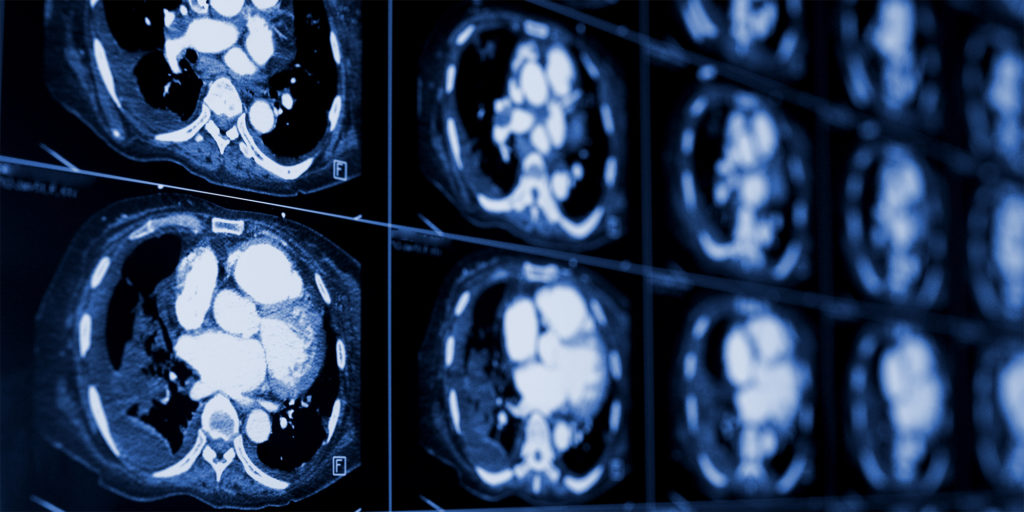
CT scans are better at predicting a middle-aged person’s risk for a heart disease, such as a heart attack, than genetics, reports a new Northwestern Medicine study published in JAMA.

“Finding the best way to identify who is at risk for developing heart disease can help determine what needs to be done to lower their risk,” said lead study author Sadiya Khan, ’09 MD, ’14 MSc, ’10, ’12 GME, assistant professor of Medicine in the Division of Cardiology and of Preventive Medicine and a Northwestern Medicine cardiologist. “This finding can help doctors and patients in managing risk for heart disease, which is the leading cause of death in the U.S.”
Currently, conventional measures of risk-factor levels, such as blood pressure and cholesterol, are used by doctors to determine a person’s likelihood of developing coronary heart disease or blockages of the arteries in the heart. But some people may experience a heart attack, or related heart problem, without one of those conventional factors picking it up.
Because the risk for heart disease can be inherited, scientists were optimistic that a person’s genetics can inform who is at greatest risk, Khan said. It was posited that polygenic risk scores — a compilation of more than 6 million commonly occurring genetic variants associated with heart disease — could be used as a potential breakthrough for personalized medicine.
But the new Northwestern study directly compares genetics and CT scans for coronary artery calcium and demonstrates that the CT scan does a better job than genetics at predicting risk for heart disease in middle age.
“These findings support recommendations to consider CT screening to calculate risk for heart disease in middle-aged patients when their degree of risk is uncertain or in the intermediate range,” Khan said.
The study used data from 3,208 adults from two cohort studies, one based in the U.S. and one in Rotterdam in the Netherlands. Investigators used data on risk factors for heart disease (smoking status, cholesterol levels, blood pressure), genetics and CT scan data to estimate the risk of developing heart disease. The study included data from patients with up to 17 years of follow-up.
The investigators looked at how using either CT scans or polygenic risk scores affected the risk predicted of individuals based on conventional risk factors – blood pressure and cholesterol, and whether the addition of either of these markers (CT or genetics) put them in a different risk category. Low risk means someone has less than a 7.5 percent risk of developing heart disease in the next 10 years. If it’s above 7.5 percent, statins are recommended.
Using genetic data did not affect a person’s risk category based on their conventional risk factors (blood pressure and cholesterol.) But only when considering CT scan, half the study participants moved into the high-risk group.
“The data from the CT scan can help identify individuals who may benefit from medications, such as statins, to reduce their risk of heart disease,” Khan said.
Other Northwestern authors are Norrina Allen, PhD, the Quentin D. Young Professor of Health Policy in the Department of Preventive Medicine; Donald Lloyd-Jones, MD, ScM, the chair and Eileen M. Foell Professor of Preventive Medicine; and Philip Greenland, MD, the Harry W. Dingman Professor of Cardiology.
The study was supported by grant R01HL159250 from the National Heart, Lung, and Blood Institute of the National Institutes of Health.






