This article was originally published in the Breakthroughs Newsletter. Find more stories like this, as well as the Breakthroughs Podcast, on the Breakthroughs homepage.
As far as viruses go, human immunodeficiency virus (HIV) is quite simple. About 100,000 times smaller than a red blood cell, the virus expresses just a dozen proteins, yet it can establish a lifelong infection that, if left untreated, causes acquired immunodeficiency syndrome (AIDS) and death. At Feinberg, HIV science ranges from examining microscopic mechanisms of initial infection to trials of treatments, all pointed towards the goal of ending one of the world’s largest pandemics.

“It’s been amazing to see science and medicine work to produce these improvements,” said Thomas Hope, PhD, professor of Cell and Developmental Biology and of Obstetrics and Gynecology. “We are seeing a new generation of scientists enter the field, and those new perspectives will help us solve this problem.”
Identifying Microscopic Mechanisms
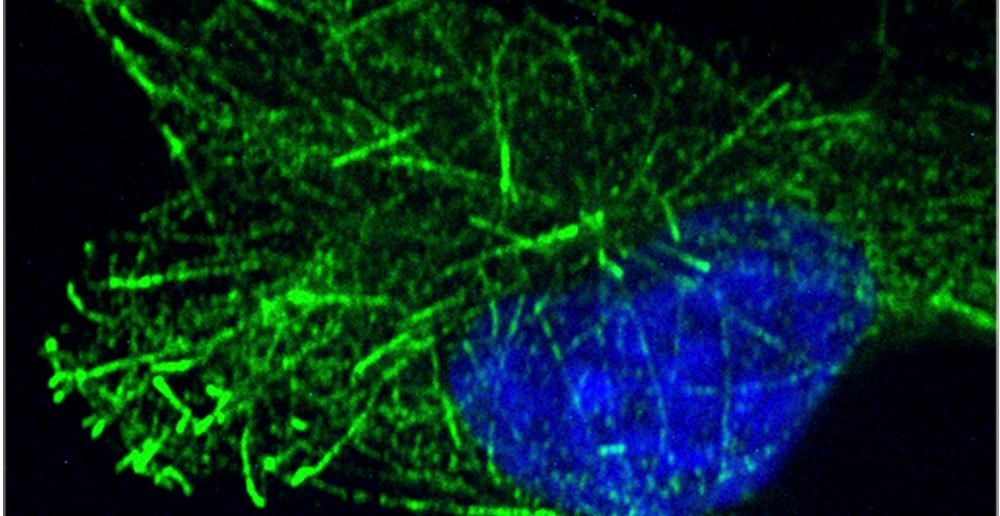
Many viruses exploit microtubule filaments in host cells, traveling along these “highways” to reach the virus’s preferred replication site within a cell. Mojgan Naghavi, PhD, professor of Microbiology-Immunology, has shown that HIV uses some unusual strategies to do so; an HIV capsid mimics a central microtubule regulator to control its transport and disassembly (commonly called uncoating), according to recent studies published in The EMBO Journal and Proceedings of the National Academy of Sciences (PNAS). This allows the virus to coordinate transport, uncoating and converting its RNA genome to a DNA form on the way to the nucleus, where it then integrates into the host cell genome.
“More refined drugs targeting highly specialized microtubule regulators could potentially be an attractive approach for development of new, non-toxic therapeutic strategies to treat HIV,” Naghavi said.

This mechanism is one example of how HIV “hijacks” native processes in cells and uses them replicate and spread. HIV is remarkably resourceful, according to Judd Hultquist, PhD, assistant professor of Medicine in the Division of Infectious Diseases, who studies how the virus manipulates host cell machinery to replicate.
In a recent study published in Nature Communications, Hultquist and his collaborators used a CRISPR-Cas9 gene editing approach to ablate over 400 different genes in CD4+ T cells isolated from human blood donors. By challenging these cells with HIV in the lab, they were able to identify 86 host factors that the virus uses to replicate. While nearly half of these have been studied previously, the other half represent new targets for mechanistic study, Hultquist said.
Studying the myriad ways in which HIV infects cells and alters their normal functioning is critical for developing better treatments and an eventual cure, according to Hultquist.
“If we’re going to build a drug with curative potential, it has to be able to eliminate or disable the virus in all of the places it may be lurking throughout the body,” Hultquist said.
The persistence of the virus is the main reason efforts to cure HIV have so far proven unsuccessful, according to Hope. Even with antiretroviral therapy (ART) that can reduce levels of virus to undetectable levels, as soon as somebody stops taking those medications, the virus can bounce back. Hope has spent the last two years searching for HIV “reservoirs,” the locations in the body where virus remains even after treatment.
“Everyone looks in the blood, but the virus is only detected in the blood about a week or so after infection,” Hope said. “To find a cure, we need to find these reservoirs where infection is happening first and where the virus is hiding out.”
Developing Better Treatment
The last three decades have seen significant improvements in treatment options for HIV, but life expectancy for people with HIV is still shorter compared to other people. Due to a phenomenon of premature aging, people with HIV experience high rates of cardiovascular disease, dementia and bone loss.

Frank Palella, MD, the Potocsnak Family – C.S.C. Professor of Medicine in the Division of Infectious Diseases, was recently named associate director of Northwestern’s new Potocsnak Longevity Institute and director of the institute’s Potocsnak Center for Aging and HIV. The institute will address the special needs of persons aging with HIV through research, education and patient care, according to Palella.
Northwestern is also involved in improving therapies. The classic three-drug ART regimen worked well, but advancements in the medications themselves now allow for a two-drug regimen. Babafemi Taiwo, MBBS, the Gene Stollerman Professor of Medicine and chief of Infectious Diseases in the Department of Medicine, led the AIDS Clinical trial Group (ACTG) study published in the journal Clinical Infectious Disease that first showed efficacy of this new treatment strategy.
“This heralds a shift in the three-drug paradigm as a way to lower lifetime exposure to these medications,” Taiwo said. “We know this can be done successfully without compromising suppression.”
Increasing the duration of these treatments is another priority, as most regiments require daily medication that can complicate adherence or serve as a constant reminder of one’s HIV infection. Current efforts include long-acting pre-exposure prophylaxis or ART that could mitigate these issues and increase treatment adherence.
Future of HIV
The COVID-19 pandemic forced science and medicine to marshal collective resources against an emerging threat, which could pay dividends for infectious diseases beyond COVID-19. Of particular interest are advancements such as the mRNA vaccines, which have proven effective against SARS-CoV-2, but are yet to be tested against a virus that mutates and changes as rapidly as HIV, according to Hultquist.
“The pandemic loosened up the wheels in terms of getting these big ideas tested and tried,” Hultquist said. “It also precipitated a historic investment in virus research, and this has enabled us to bring together scientists across diverse disciplines who may have never even thought about viruses before, and here we all are working towards one common goal.”
Further, several patients with HIV have received stem cell transplants to treat cancer and have been cured of the virus. While this treatment is unfeasible on a larger scale, it provides a blueprint for how scientists might one day design a cure for HIV, according to Taiwo.
“We’re learning a lot from these patients,” Taiwo said. “We now know biological markers of cure, and we have a general strategy. But most importantly; we know it’s possible.”
Hope, Naghavi and Taiwo are members of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.






