
Northwestern Medicine scientists have discovered that a protein called mDia2 is vital for one step of bone marrow transplantation, according to a study published in Nature Communications.
Boosting mDia2 function in transplanted bone marrow cells — known as hematopoietic stem and progenitor cells (HSPCs) — could one day lead to more efficient transplantation, which is used to treat a variety of blood diseases such as sickle cell anemia, leukemia and lymphoma.
“Oftentimes you have to use a lot of stem cells to treat the patient, and many transplanted stem cells got stuck in the vasculature” said Peng Ji, MD, PhD, GME ’15, ’17, associate professor of Pathology in the Division of Hematopathology and senior author of the study. “This could make it easier for stem cells to migrate out of the vasculature, so the patients will have an increased rate of successful transplantation.”
Bone marrow transplantation infuses HSPCs into patients with damaged or diseased bone marrow. These HSPCs give rise to other blood cells, replenishing bone marrow in the patient.
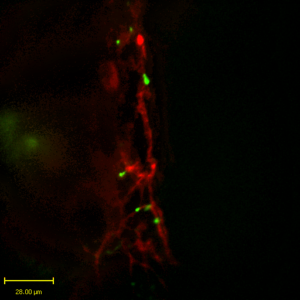
After injection, these HSPCs must first “home in” on the bone marrow vasculature, entering and traveling through these blood vessels to their destination within the bone. There, they migrate out of the blood vessels and graft to the “niche,” small carve-outs in the interior of the bone. This process of migration and grafting is known as engraftment.
While the proteins and factors important for grafting into the niche are well-established, what controls migration out of the blood vessels has been less studied, according to Ji.
“This trans-endothelial migration process was very unclear,” said Ji, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
One potential influence on migration was mDia2, a protein that is known to be important in red blood cells and in HSPCs. To investigate, Ji, along with Yang Mei, PhD, a postdoctoral fellow in the Ji laboratory and lead author of the study, performed an experiment that replicated the conditions of a bone marrow transplant in mouse models.
The scientists knocked out mDia2 in a population of mice, then took those mDia2-negative HSPCs and transplanted them into normal mice, comparing the results of the transplantation with a control. They found that mDia2-negative donor cells were less efficient and took longer to graft to the niche when compared to the control.

Closer examination revealed that while the mDia2-negative HSPCs were correctly targeting on the bone marrow vasculature, they were mostly unable to migrate out of the blood vessel.
“This let us know that the main function of mDia2 is to migrate cells out of the vasculature,” Ji said.
Bone marrow transplantation is an effective treatment but can require large volumes of blood and stem cells to be useful. Boosting mDia2 through the use of a small-molecule agonist could reduce the volume of blood required for treatment and increase the success rate of transplantation, Ji said.
“We can probably add some of this agonist and facilitate migration of these cells out of the vasculature,” Ji said. “This is a promising future direction for study.”
This work was supported by National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) grants R01-DK102718 and R01-DK124220, National Heart, Lung, and Blood Institute grant R01-HL148012 and Department of Defense grant CA140119 and CA180214.






