A special COVID-19 testing team has been put in place at Northwestern, with the goal of at least quadrupling the number of tests processed at Northwestern Medicine hospitals — from about 90 per day to more than 350 per day — and in the process, greatly reducing test result turnaround times.
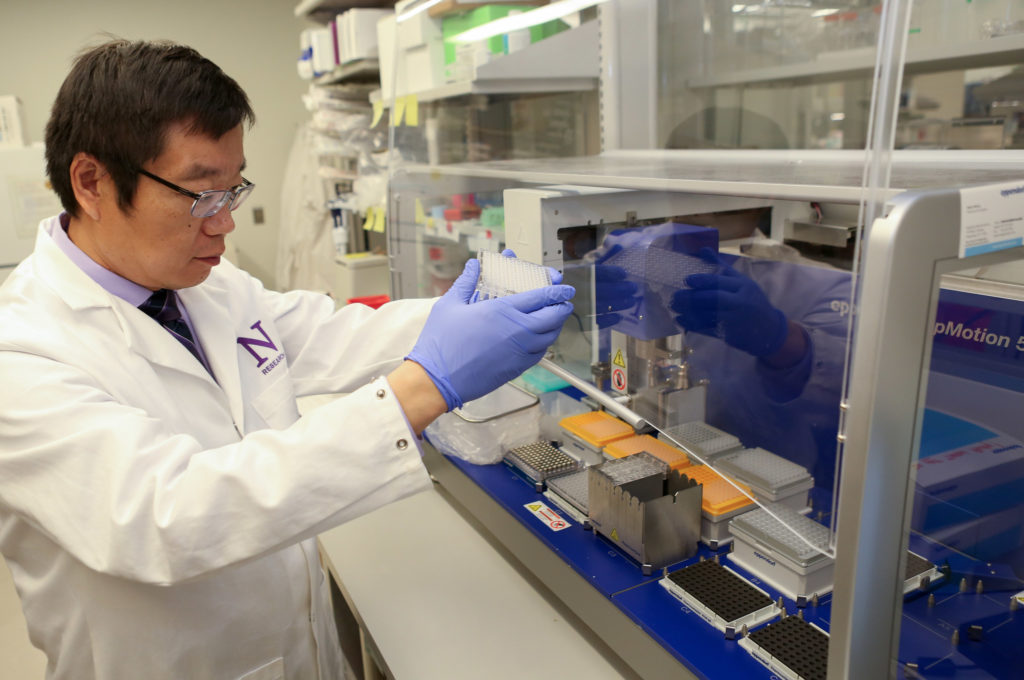
Six medical school research staff have been trained and are now working in shifts to address the need, with the effort being led by Xinkun Wang, PhD, director of the NUSeq Core Facility in the Center for Genetic Medicine and research associate professor of Biochemistry and Molecular Genetics.
In the Q&A below, Wang details the effort and how it will help meet the urgent need to deploy more widespread COVID-19 testing.
How is NUSeq Core supporting COVID-19 testing at Northwestern Medicine?
Not having enough testing capacity for COVID-19 has been a major issue. Hospitals were allowed to build and use their own COVID-19 tests after an FDA announcement on February 29. Northwestern Medicine established a test for the virus in the second week of March. This test looks for COVID-19 virus by testing for the virus RNA, or genetic material. Northwestern Medicine was able to conduct 90 tests per day but needed to be able to do more tests.
NUSeq, which operates under the Center for Genetic Medicine, responded to this need by setting up a testing site to help the health system increase testing capacity and cut turnaround time. The NUSeq site uses the exact same testing protocol that the Northwestern Medicine testing lab developed, and is doing this under the supervision of the health system’s clinical lab and FDA authorization. For this coordinated operation, NUSeq staff picks up patient samples from the hospital and brings to NUSeq for testing. The testing data is then sent back to the health system for analysis and reporting.
What machinery, tools and skills are being used?
A major part of this operation requires BioSafety Cabinets (BSCs). These are large containment devices used by laboratories that work with infectious pathogens. They help protect the testing staff from contracting pathogens in patient samples. These are the hoods that you often see researchers working in front of wearing gloves and other protective gear.
With help from Basic Science Administration (BSA), led by a team headed by Matt Temkin and Feinberg’s Department of Pathology, we mobilized three BSCs for the NUSeq testing site. These BSCs are used for the first phase of the testing protocol. This first step extracts RNA from patient swab samples. The second phase is making a copy of the viral RNA into DNA. The DNA is then used for a step called real-time quantitative polymerase chain reaction (PCR). For setting up real time quantitative PCR, the Thorson Goodall Diagnostic Molecular Biology (DMB) laboratory at Northwestern Memorial Hospital provided NUSeq with a PCR cabinet to help avoid potential contamination from other sources.
The PCR process is carried out using NUSeq’s two real-time quantitative PCR machines. Many of these steps are done manually and this required training the staff on the specifics of the health system’s clinical lab protocol. For a clinical test like this, it is essential that the FDA-approved protocol is strictly followed.
How did this partnership come about?
Over the weekend of March 14, Ken Hedley, vice president of operations at Northwestern Medicine and Gary Noskin, MD, chief medical officer at Northwestern Memorial Hospital and professor of Medicine in the Division of Infectious Diseases, began inquiring about the possibility of using Feinberg research labs to help with RNA extraction and PCR. This was because the research labs routinely use these steps in experiments. After discussions between Ali Shilatifard, PhD, the Robert Francis Furchgott Professor and chair of Biochemistry and Molecular Genetics; Marc Mendillo, PhD, assistant professor of Biochemistry and Molecular Genetics and Elizabeth McNally, MD, PhD, the Elizabeth J. Ward Professor of Genetic Medicine, professor of Medicine in the Division of Cardiology and director of the Center for Genetic Medicine (CGM), we focused on NUSeq, the core facility which I direct.
At this core, staff routinely conducts all types of DNA and RNA analysis. As part of its mission, NUSeq provides highly accurate and reproducible sequence analysis and these rigorous standards made NUSeq the logical response unit for the health system’s request. By Sunday, March 15, the wheels were in motion to convert NUSeq into a facility to make this a reality. Rex Chisholm, PhD, the Adam and Richard T. Lind Professor of Medical Genetics and vice dean for Scientific Affairs and Graduate Education, and Hedley began gathering the necessary information and I reviewed NUSeq’s available equipment and conferred with staff about helping. Everyone was on board.
What hurdles did you have to cross to get the testing site up and running?
CLIA (Clinical Laboratory Improvement Amendments) certification is required for clinical testing laboratories. Northwestern Medicine clinical laboratories operate under CLIA certification, so the first step was to extend that CLIA certification to NUSeq. This required approval by the State of Illinois. We also needed to have approval from the Northwestern Office of Research Safety, which was expeditiously handled by Andrea Hall, PhD, its director.
We also needed to have the BSCs in place and all the equipment certified, which was challenging given that campus had been closed to all visitors. Luckily and with steady input from Rex Chisholm, Robert Valadka, associate director of facilities, the Basic Science Administration (BSA) team, the Office of Research Safety, the Department of Pathology, and countless others, we were able to get protocols in place and equipment installed and properly certified. Northwestern Medicine hospitals also provided personal protective equipment (PPE) such as gowns and gloves. As has been noted in the lay press, the lack of N95 face masks was a major hurdle we had to overcome. The BSA team again stepped in and helped identify secure a vendor identified by BSA’s procurement team. Research Safety also provided a batch of N95 masks donated by the Northwestern University community. These steps all came together over about 10 days, including two weekends, a remarkable feat!
How many Feinberg staff are working on this testing?
There are currently six staff in total, three from NUSeq (Alan Aalsburg, Laura Shihadah and Shaneh Zarinebaf), three from the rest of CGM (Katherine Fallon, Nina Reiser, and Lauren Vaught). They are all proficient on the COVID-19 testing protocol and listed on the Northwestern Medicine CLIA testing personnel roster. Thanks to their voluntary contribution, Northwestern Medicine is able to catch up with the testing.
It should be noted that a number of research groups at Feinberg and other Northwestern schools reached out wanting to help, and these offers of support were very much appreciated. The support, donation, and encouraging words the team receives from the Feinberg and the Northwestern University community have been very inspiring for the team to work harder to combat the virus.






