Northwestern Medicine scientists discovered how damage to certain brain regions can contribute to amnesia, according to a study recently published in Nature Communications.
Mapping previously unknown connections within the brain, the investigators identified a memory encoding circuit that helps explain why some damage outside of the central memory-encoding region — called the hippocampal complex — can cause memory impairment, according to Jordan Grafman, PhD, professor of Physical Medicine and Rehabilitation, of Psychiatry and Behavioral Sciences and co-author of the study.
“This indicates that the key brain hub for memory encoding has direct connections to other nodes in a brain circuit that contributes to memory encoding, representation and storage,” said Grafman, who is also a professor in the Ken and Ruth Davee Department of Neurology. “It is important to investigate memory circuits, since identifying a key circuit allows researchers and clinicians to identify other features, including its chemistry, genetics and cognitive or emotional functions that are unique to the nodes in the circuit beyond that of the main hub, in this case the hippocampal complex.”
In the study, Grafman and his collaborators searched their database to identify patients who had experienced strokes or Vietnam War veterans who suffered penetrating brain injuries in combat. This review produced 53 lesion locations that caused amnesia or profound memory loss, according to the study.
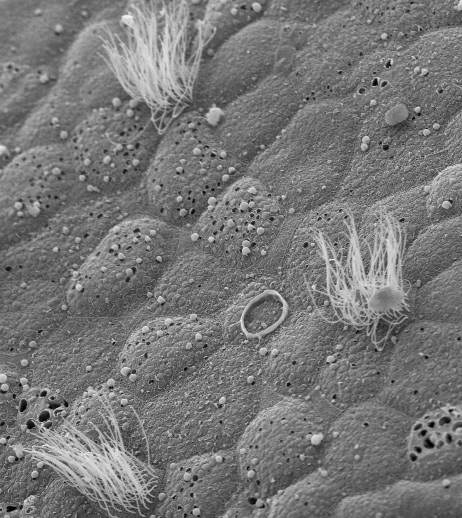
Once they had a set of locations, the investigators used human connectome data to identify where neurons at these locations projected out to, finding many of these 53 locations had tendrils snaking towards the same place: the subiculum-retrosplenial continuum located in and near the hippocampal complex, which is a part of the circuit of Papez.
Each neuron in the human brain is connected to up to 10,000 others, and a brain circuit is the path that electrical activity follows as it moves from one nerve cell to the next. First described in 1937, the circuit of Papez includes parts of the hippocampus, thalamus and hypothalamus.
This marks the first time that certain nodes outside of the main circuit of Papez have been linked to human memory in a causal fashion because of that connectivity, according to Grafman, and further lesion studies could have wide-ranging benefits.
“This allowed us to infer that all the damaged regions in our stroke and penetrating traumatic brain-injured patients that caused severe memory deficits were commonly connected to a key memory region deeper in the brain,” Grafman said. “Any time you can better specify the brain regions concerned with certain functions, you can develop more sensitive and specific tests to evaluate the brain’s functions leading to earlier and more precise diagnoses. This can improve the targeting of medical and behavioral interventions to help patients with brain disorders and injury, and moving into the future, provide better interfaces between devices designed to assist people to function better and the brain areas those devices interact with.”