A treatment of inhaled inorganic nitrite did not improve exercise capacity among patients with a common form of heart failure, according to the results of a clinical trial published in JAMA.
Sanjiv Shah, ’00 MD, the Neil J. Stone, MD, Professor of Medicine in the Division of Cardiology, was a co-author of the study.
About half of all cases of heart failure are classified as heart failure with preserved ejection fraction (HFpEF), a condition where the heart is pumping normally but is abnormally stiff. HFpEF is associated with significant morbidity and mortality, and there are currently no effective treatments.
Previous research had suggested that impairments in the nitric oxide pathway may play an important role in the progression of HFpEF. Furthermore, small studies have demonstrated that short-term administration of inorganic nitrite strengthens nitric oxide signaling, which may in turn improve exercise capacity among patients with HFpEF.
However, inorganic nitrite had never been tested with longer-term use or in a larger, multi-center trial.
In the current study (the INDIE-HFpEF trial), 105 patients with HFpEF at 17 U.S. sites were randomized to receive either inhaled inorganic nitrite or a placebo for four weeks, followed by a crossover to the alternate treatment for an additional four weeks. Investigators then assessed the participants’ exercise capacity (as measured by peak oxygen consumption).
They found that there was no significant difference in exercise capacity between the patients who received the inorganic nitrite and those who received the placebo.
There were also no significant differences in daily activity levels, or other secondary endpoints of the trial, including health-related quality of life scores and clinical measures of heart function.
“The lack of a benefit with inhaled nitrite in the INDIE-HF trial does not necessarily mean that this class of drugs is ineffective in HFpEF,” Shah explained. “Alternate delivery methods, including oral forms of the drug (which are likely longer acting), are currently being tested and may ultimately show a benefit in improving exercise capacity in HFpEF.”
The INDIE-HFpEF investigators note that exercising training is the only intervention that has consistently been shown to improve aerobic capacity in HFpEF, and suggest that future trials may need to incorporate exercise or weight loss in order to achieve improvements.
The JAMA study was supported by the Heart Failure Clinical Research Network, which is supported by the National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) grants U10 HL084904, U10 HL110312, U10 HL110337, U10 HL110342, U10 HL110262, U10 HL110297, U10 HL110302, U10 HL110309, U10 HL110336, and U10 HL110338, and Savara Therapeutics, which manufactures the inorganic sodium nitrite.
Automating Cardiac Imaging With Deep Machine Learning and Artificial Intelligence
Shah was also a co-author of a recent study, published in the journal Circulation, that described a pipeline for the automated interpretation of echocardiograms, using cutting-edge deep machine learning and computer vision techniques.
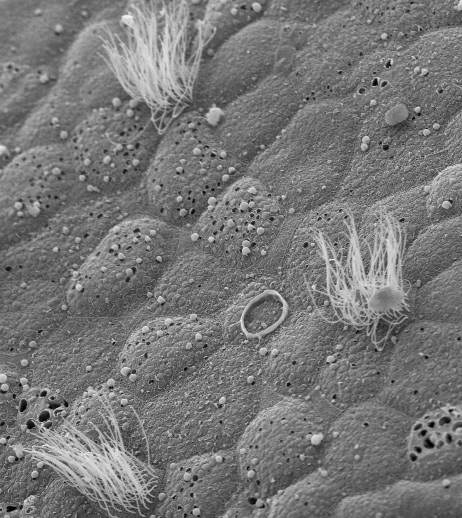
Echocardiograms and other forms of cardiac imaging can help detect early signs of heart disease, but currently require specialists to administer these tests and evaluate the images. An automated method of interpretation could “democratize echocardiography,” the authors wrote, helping to bring imaging to primary care settings and rural areas, while slashing healthcare costs. A more standardized and accelerated method of analysis could also benefit future research.
“Automated, machine learning-based cardiac imaging could also lead to earlier diagnosis of treatable cardiomyopathies (heart muscle diseases) such as cardiac amyloidosis, an often missed diagnosis in which proteins build up in the heart muscle and cause the heart to not work properly, leading to congestive heart failure,” Shah explained.
In the paper, the team of scientists employed recent advances in deep machine learning and computer vision algorithms to develop a pipeline for the interpretation of cardiac structure, function and disease detection. They further demonstrated the accuracy and scalability of the method through the evaluation of more than 14,000 echocardiograms.
The Circulation study was supported by NIH/NHLBI grant DP2 HL123228. Additional funding for a portion of the echocardiographic data used for validation was provided by NIH/NHLBI grant R01 HL127028 and National Institutes of Health/National Institute for Diabetes and Digestive and Kidney Diseases grant P30DK090868.
Shah and the senior author of the paper, Rahul Deo, MD, PhD, of Brigham and Women’s Hospital and also an adjunct associate professor of Preventive Medicine at Northwestern, recently received funding from the National Institutes of Health as co-principal investigators of a four-year research project to further the science of automating cardiac imaging (R01 HL140731).