Pathways in the brain work together to excite and inhibit nerve cells that control movement, but this process goes awry in Parkinson’s disease. A new Northwestern Medicine study reveals that excessive brain plasticity in the subthalamic nucleus may be pivotal to abnormal brain activity and impaired movement in Parkinson’s disease, revealing a novel therapeutic target.
Plasticity is an ongoing process in which the brain’s neuronal pathways adapt to change – for example, learning something new or recovering from an injury. The study, published January 8 in Neuron, demonstrates that in Parkinson’s disease, the brain responds to losing dopamine neurons with an abnormal, maladaptive level of plasticity that promotes pathological activity.
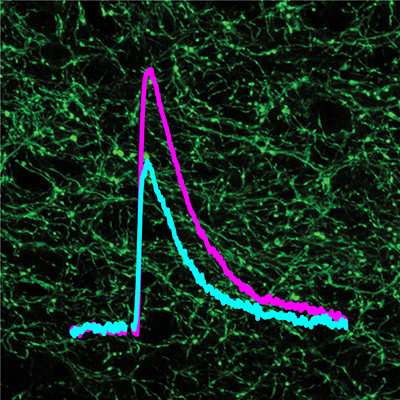
In Parkinson’s disease, degeneration of dopamine neurons compromises the brain’s ability to encode and process information, leading to reduced movement, rigidity and tremor. The symptoms of Parkinson’s disease are associated with abnormally synchronous brain activity in the cerebral cortex and deeper structures called the subthalamic nucleus and globus pallidus. Until now, scientists didn’t know what causes these structures to become synchronized in Parkinson’s disease.
“The subthalamic nucleus has long been implicated in the expression of Parkinson’s disease symptoms and is a common therapeutic neurosurgical target,” said senior author of the study Mark Bevan, PhD, professor in Physiology. “We found that the nucleus possesses an intrinsic plasticity mechanism that regulates the balance of excitatory cortical and inhibitory pallidal nerve cell inputs.”

In the study, Bevan and collaborators discovered that after loss of dopamine, increased excitation of the subthalamic nucleus by the cortex led to excessive strengthening of synchronizing pallidal inputs.
“After dopaminergic nerve cells are destroyed in animal models of Parkinson’s disease, it takes several weeks for abnormal brain activity – identical to that seen in Parkinson’s disease patients – to develop,” Bevan said. “This finding argues that it’s not the acute loss of dopamine that causes abnormal activity; it’s the fact that the loss of dopamine triggers maladaptive plasticity in the affected brain areas.”
Now that scientists have uncovered this process of abnormal plasticity in the subthalamic nucleus, they can target it in continuing research.
“So far, everything we’ve done suggests that the plasticity we’re seeing in this tiny brain nucleus is really important. When we prevent or compensate for it, we observe a remarkable improvement in terms of function,” Bevan said.
This study was funded by National Institutes of Health (NIH) National Institute of Neurological Disorders and Stroke grants 2R37 NS041280, 2P50 NS047085 and P30 NS054850.






