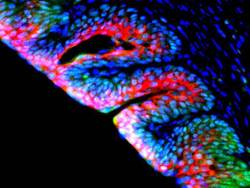
Using a novel approach that capitalizes on the potential of two distinct cell populations transplanted from a person’s bone marrow, Arun K. Sharma, PhD, research assistant professor in urology, was able to regenerate bladder tissue. (pictured here)
A new approach to bladder regeneration is capitalizing on the potential of two distinct cell populations harvested from a patient’s healthy bone marrow.
The Northwestern Medicine® research, published in the Proceedings of the National Academy of Sciences by Arun K. Sharma, PhD, research assistant professor in urology, and colleagues, is an alternative to contemporary tissue-engineering strategies. The bone marrow cells are being used to recreate the organ’s smooth muscle, vasculature, and nerve tissue.
“We are manipulating a person’s own disease-free cells for bladder tissue reformation,” said Sharma, a member of the Institute for BioNanotechnology in Medicine and Ann & Robert H. Lurie Children’s Hospital of Chicago Research Center. “We have used the spina bifida patient population as a proof of concept model because those patients typically have bladder dysfunction. However, this regeneration approach could be used for people suffering from a variety of bladder issues where the bone marrow microenvironment is deemed normal.”

In end-stage neurogenic bladder disease – an illness often associated with spinal cord diseases like spina bifida – the nerves which carry messages between the bladder and the brain do not work properly, causing an inability to pass urine. The most common surgical option, augmentation cystoplasty, involves placing a “patch” derived from an individual’s bowel over a part of the diseased organ in order to increase its size. The current “gold standard,” the procedure remains problematic because the bowel tissue introduces long-term complications like the development of electrolyte imbalance and bladder cancer.
Because Sharma’s procedure does not use bowel tissue, it offers the benefits of augmentation without the association of long-term risks. His technique combines stem and progenitor cells from a patient’s bone marrow with a synthetic scaffold created in the lab of Guillermo Ameer, ScD, professor of biomedical engineering and surgery. The scaffold takes the place of the traditional patch.
“We decided to use material that has the ability to be tailored to simulate mechanical properties of the bladder,” said Sharma, director of pediatric urological regenerative medicine at Lurie Children’s. “Using the elastomer created by Dr. Ameer and the bone marrow stem and progenitor cells, I believe that we have developed a technique that can potentially be used in lieu of current bladder augmentation procedures. However, further study is needed.”
Sharma says he now plans to test the procedure in larger animal models. His initial research was supported in part by an Excellence in Academic Medicine grant funded by the Illinois Department of Healthcare and Family Services.






