Human Stem Cells Transformed Into Neurons Lost In Alzheimer’s
Northwestern Medicine researchers for the first time have transformed a human embryonic stem cell into a critical type of neuron that dies early in Alzheimer’s disease and is a major cause of memory loss.
This new ability to reprogram stem cells and grow a limitless supply of the human neurons will enable a rapid wave of drug testing for Alzheimer’s disease, allow researchers to study why the neurons die and could potentially lead to transplanting the new neurons into people with Alzheimer’s.
The paper will be published March 4 in the journal Stem Cells.
These critical neurons, called basal forebrain cholinergic neurons, help the hippocampus retrieve memories in the brain. In early Alzheimer’s, the ability to retrieve memories is lost, not the memories themselves. There is a relatively small population of these neurons in the brain, and their loss has a swift and devastating effect on the ability to remember.
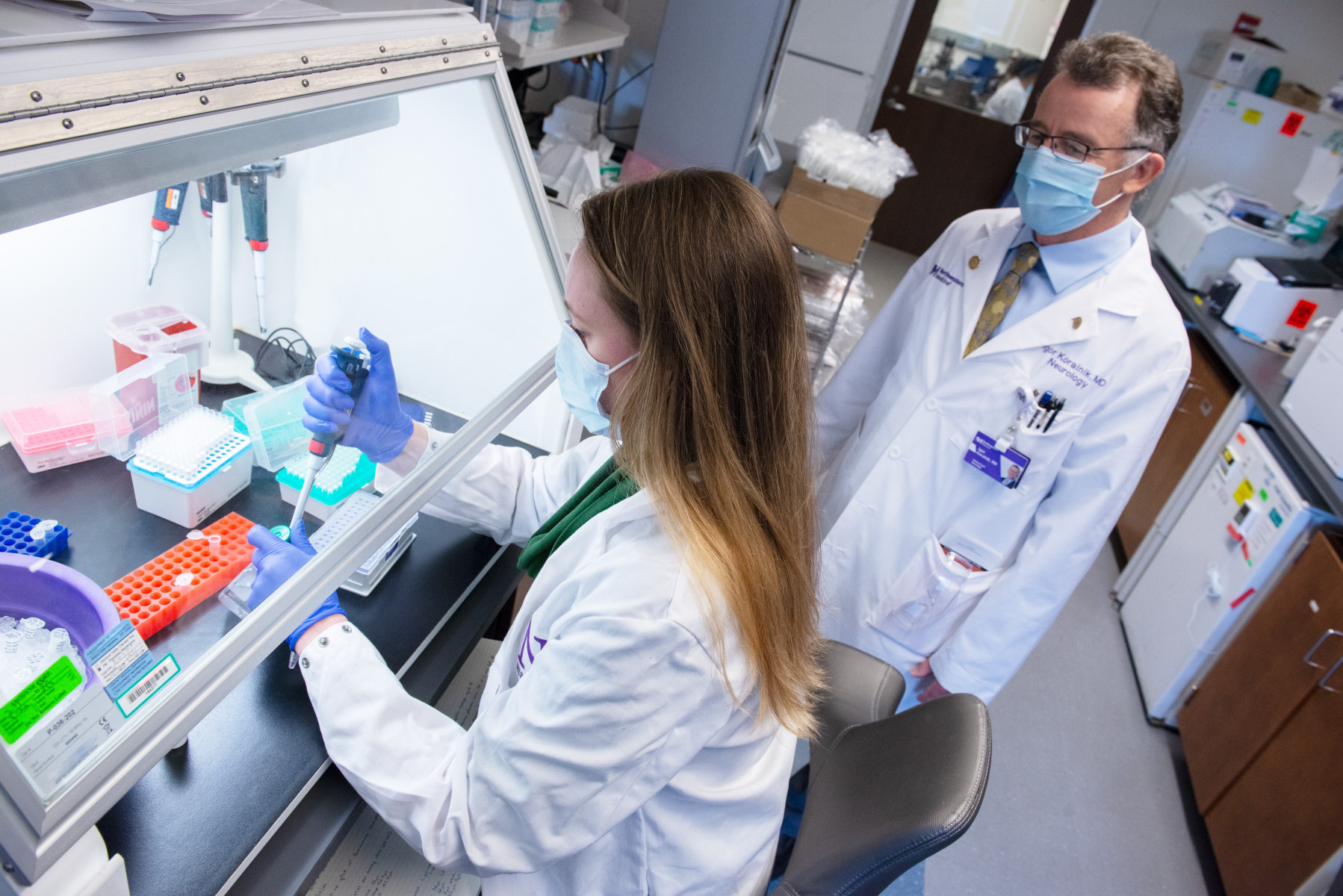
“Now that we have learned how to make these cells, we can study them in a tissue culture dish and figure out what we can do to prevent them from dying,” said senior study author Jack Kessler, MD, chair of neurology and the Davee Professor of Stem Cell Biology at Northwestern University Feinberg School of Medicine and a physician at Northwestern Memorial Hospital.
The lead author of the paper is Christopher Bissonnette, a former doctoral student in neurology who labored for six years in Kessler’s lab to crack the genetic code of the stem cells to produce the neurons. His research was motivated by his grandfather’s death from Alzheimer’s.
“This technique to produce the neurons allows for an almost infinite number of these cells to be grown in labs, allowing other scientists the ability to study why this one population of cells selectively dies in Alzheimer’s disease,” Bissonnette said.
The ability to make the cells also means researchers can quickly test thousands of different drugs to see which ones may keep the cells alive when they are in a challenging environment. This rapid testing technique is called high-throughput screening.
Kessler and Bissonnette demonstrated the newly produced neurons work just like the originals. They transplanted the new neurons into the hippocampus of mice and showed the neurons functioned normally. The neurons produced axons, or connecting fibers, to the hippocampus and pumped out acetylcholine, a chemical needed by the hippocampus to retrieve memories from other parts of the brain.
Human Skin Cells Transformed Into Stem Cells And Then Neurons
In new, unpublished research, Northwestern Medicine scientists also have discovered a second novel way to make the neurons. They made human embryonic stem cells (called induced pluripotent stem cells) from human skin cells and then transformed these into the neurons.
Scientists made these stem cells and neurons from skin cells of three groups of people: Alzheimer’s patients, healthy patients with no family history of Alzheimer’s, and healthy patients with an increased likelihood of developing the disease due to a family history of Alzheimer’s because of genetic mutations or unknown reasons.
“This gives us a new way to study diseased human Alzheimer’s cells,” Kessler said. “These are real people with real disease. That’s why it’s exciting.”
Researcher Motivated By His Grandfather’s Alzheimer’s Disease
Bissonnette’s persistence in the face of often frustrating research was fueled by the childhood memory of watching his grandfather die from Alzheimer’s.
“I watched the disease slowly and relentlessly destroy his memory and individuality, and I was powerless to help him,” Bissonnette recalled. “That drove me to become a scientist. I wanted to discover new treatments to reverse the damage caused by Alzheimer’s disease.”
“My goal was to make human stem cells become new, healthy replacement cells so that they could one day be transplanted into a patient’s brain, helping their memory function again,” he said.
Bissonnette had to grow and test millions of cells to figure out how to turn on the exact sequence of genes to transform the stem cell into the cholinergic neuron.
“A stem cell has the potential to become virtually any cell in the body, from a heart cell to a layer of skin,” he explained. “Its development is caused by a cascade of things that slowly bump it into a final cell type.”
But it wasn’t enough just to develop the neurons. Bissonnette then had to learn how to stabilize them so they lived for at least 20 days in order to prove they were the correct cells.
“Since this was brand new research, people didn’t know what kind of tissue culture mature human neurons would like to live in,” he said. “Once we figured it out, they could live indefinitely.”
The research was supported by the National Institutes of Health.
Members of the media, please contact Marla Paul via e-mail or at (312) 503-8928 for more information about this story.