Tissue Engineering Topic of 13th Annual Frances Feinberg Memorial Lecture
 |
|
|
Anthony Atala, MD |
More than 50 years after the first organ transplant (kidney) in Boston, the medical profession is still grappling with the same challenges â namely, organ rejection and the lack of availability, according to Anthony Atala, MD, during the Frances Feinberg Memorial Lecture, “Regenerative Medicine, Tissue Engineering and Stem Cells: New Approaches to Health Care.” A pediatric urology surgeon, Atala, founding director of the Wake Forest Institute for Regenerative Medicine and chair of the Department of Urology at Wake Forest University School of Medicine, is all too familiar with these challenges.
“The number of people on transplant lists has doubled. With our aging population, organs tend to fail more, while the number of donors has stayed the same,” the W.H. Boyce Professor said during his presentation on September 8 at the Feinberg Pavilion. “We started investigating making organs ‘to order,’ growing the patient’s own cells outside the body, so no rejection occurs.”
Atala continued, “When you look at engineering tissue to replace failing organs, there are limited options. A lot of what I do is reconstructive surgery. When we started working on this issue two decades ago for people with bladder cancer, the best choice was to replace the bladder with a piece of intestine. This was fine for patients in their 60s or 70s who had a relatively short life expectancy, but for babies with end-stage bladder disease, it was not a good option. We began asking ourselves, ‘Could we create an organ out of a patient’s own tissue as a starting point?’”
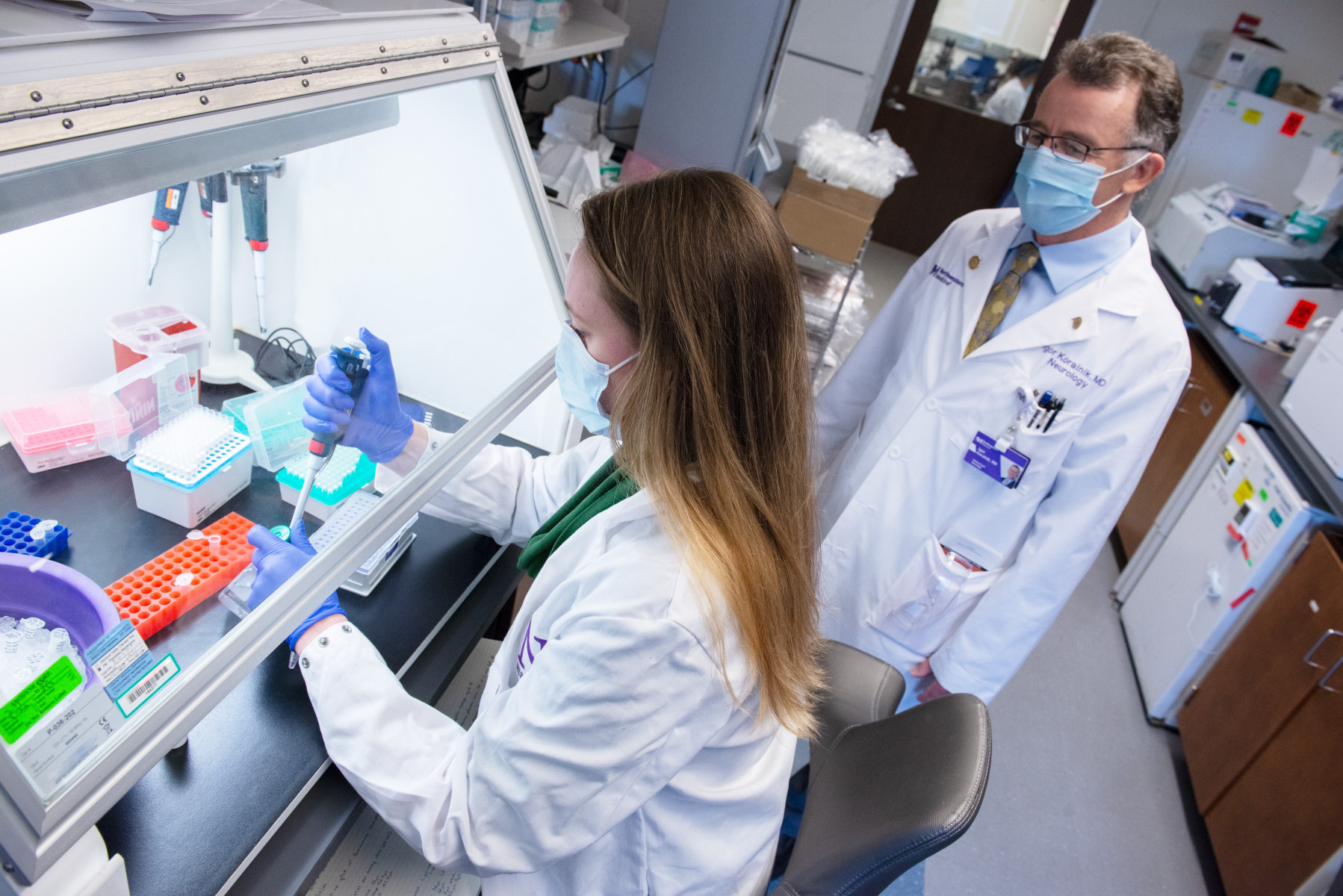
In 1981, skin was the first tissue to be engineered for a burn victim using a patient’s own cells. Years later, taking a cell sample less than half the size of a postage stamp, Atala and his group were able to engineer the first functioning organ â a bladder â for a patient with end-stage bladder failure. Using collagen molds to shape the organ structure, which was determined by X-rays, patient cells were teased apart, expanded outside the body, and then placed in three-layer molds.
“We ‘painted’ the outside of the collagen mold with muscle cells and the inside with lining cells,” he explained, “placed it in an incubator, which has the same conditions as the human body, and expanded those cells before implanting it in the patient. It’s much like baking a layer cake. As the cells form tissue, the mold dissolves, and a few months later there is a functioning organ.”
Phase 1 clinical trials were completed and the study was published in “Nature Biotechnology” in 1999. Meanwhile, the work still progresses as Atala’s team tackles the challenges of expanding the technology to larger numbers. At this stage, he is about to start Phase 3 clinical trials.
Much of Atala’s work dates back 20 years, when he began examining how to get cells to grow outside of the body. He and his team discovered what they called progenitor cells.
“These are cells found in every single tissue in our body that are ready to replicate at the time of injury. We isolated the mechanisms to harness that power to get cells to grow in large quantities. However, even in 2009, there are many primary cells that we cannot grow, and that’s where stem cells became such an important issue. ”
At Wake Forest University, they have been able to grow more than 22 tissue types, with the exception of nerve, liver, pancreas, and heart tissue.
Atala hastened to add, “The heart is a real challenge, although, there are some exciting advances being made right here at Northwestern’s Cardiovascular Research Institute under the direction of Dr. Doug Losordo.”
According to the urology surgeon, the field of regenerative medicine, which aims to recreate tissues and organs using a patient’s own cells, began in the 1920s. In 1938, the first book, “The Culture of Organs,” was published on the subject.
If this work began so long ago, it begs the question why more progress has not been made.
Atala explained, “There were very few clinical advances for many years because of the inherent challenges in how to grow and expand cells outside the body, how to deliver cells to the patient, and how to get the cells to survive once they were planted in the patient’s body.”
Unlocking these doors has enabled Dr. Atala and others to make advances, which include using porous scaffolds that look like fabric which allow cells to lay down and form sheets of tissue that enable porosity, promoting new vessel formation. In addition, Atala and his team have used bioreactors with biofeedback mechanisms that sense temperature, pH, and oxygen levels to create solid organs when total replacement is necessary. At six months, these engineered organs have the same characteristics of a normal organ, including adequate blood supply and functioning nerves .
He is quick to pay tribute to the many people across different disciplines who have been involved in making progress in this complex area.
“The work that I’ve shown you today was performed by more than 700 researchers across a 20-year span. This requires a multi-disciplinary approach between materials scientists, molecular biologists and molecular geneticists all working together to bring these technologies from the ‘bench to the bedside.’ We’ve had to go slowly and carefully to make sure the work we are doing is safe for our patients. The question we ask is, ‘Would you place this organ in your own loved ones?’”