June 26, 2007
|
Contact: Marla Paul at (312) 503-8928 or at |
|
Broadcast Media: Tamara Kerrill Field at (847) 491-4888 or at |
First Study Transplanting Angina Patients’ Purified Stem Cells Shows Safety
Researcher First Tests Cell Extraction Technique on Himself
CHICAGO—The first U.S. study to transplant a potent form of purified adult stem cells into the heart muscle of patients with severe angina provided evidence that the procedure is safe and produced a reduction in angina pain as well as improved functioning in patients’ daily lives, reports the lead researcher at Northwestern University’s Feinberg School of Medicine.
Within three to six weeks after the severe angina patients were injected with their own stem cells, many who had experienced pain just from walking to the refrigerator now only had pain when they climbed two flights of stairs.
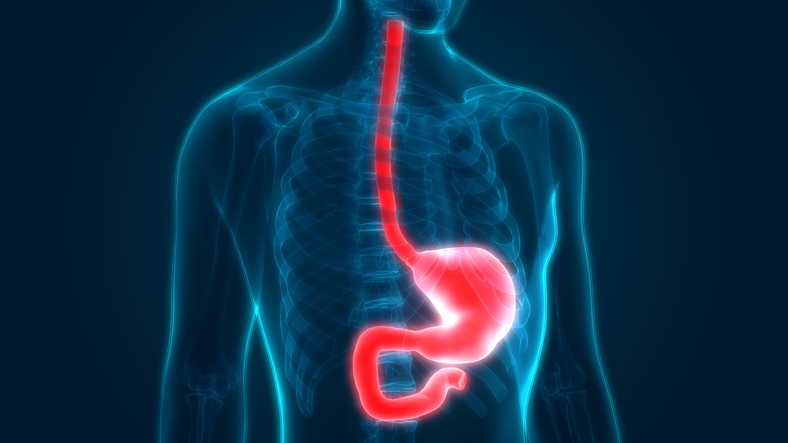
This is the first human trial in which patients’ own purified stem cells, called CD-34 cells, were injected into their hearts in an effort to spur regrowth of small blood vessels that constitute the microcirculation of the heart muscle. Researchers believe the loss of these blood vessels contributes to the pain of chronic, severe angina.
While lead researcher Douglas Losordo, MD, cautioned this was a small pilot study, he said the results are encouraging. “That’s a very meaningful change in lifestyle or functional capacity,” he noted.
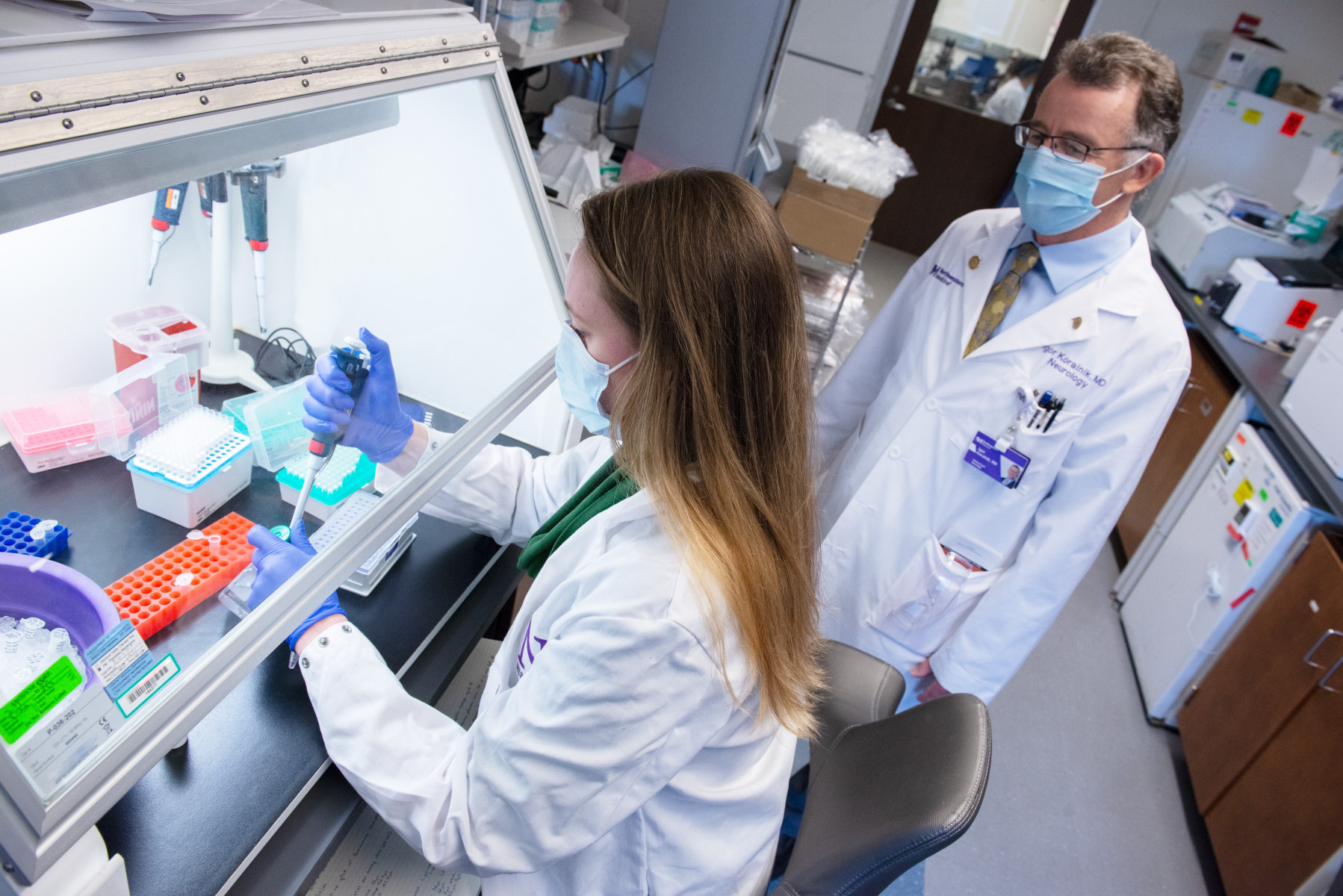
Dr. Losordo is director of the Feinberg Cardiovascular Research Institute and the Eileen M. Foell Professor of Heart Research at the Feinberg School. He also is a cardiologist at Northwestern Memorial Hospital. He conducted the research while a professor of medicine at Tufts University School of Medicine.
The primary aim of the study was to test the safety of the technique, but researchers also discovered preliminary indications of the therapy’s benefits. The new study is published in the June 26 issue of Circulation.
“Our goal is to reconstitute the microcirculation, get the blood back into the tissue, and alleviate the symptoms,” Dr. Losordo said.
Evidence in the lab shows the cell therapy appears to work in at least two ways: the CD-34 cells help to form new micro-blood vessels as well as encourage existing cells in the tissue to grow vessels, a process called neovascularization.
Of the estimated 1 million people in the United States who suffer from chronic, severe angina—chest pain due to blocked arteries—about 300,000 cannot be helped by traditional medical treatment such as angioplasty, bypass surgery, or stents. This is called intractable angina, the severity of which is designated by classes. The patients in Dr. Losordo’s study were class 3 or 4, meaning they had chest pain with normal to minimal activities such as brushing their teeth or even resting.
After the intractable angina patients were injected with their own stem cells, within three to six months many improved up to two classes in functional capability, a significant gain. The double-blind, randomized, placebo-controlled study included 24 patients ages 48 to 84.
Before Dr. Losordo launched the study with a procedure to extract stem cells from angina patients, he took the unusual step of testing the stem cell extraction procedure on himself. He took the drug patients were to take and underwent the stem cell extraction process.
“I wanted to know what the patients were going to experience,” Dr. Losordo said. “I knew it was going to be harder for the patient because I don’t have cardiovascular disease. But if it was tough for me, then there was no way I was going to subject the patients to it.”
Rather than extract the stem cells from a patient’s bone marrow, which is done in an operating room and can be a painful procedure, Dr. Losordo collected the cells from a patient’s peripheral circulation. Participants first took a drug called G-CSF for five days, which stimulates the production and release of CD-34 cells from bone marrow. An intravenous line was then inserted into a patient’s vein and the patient’s blood cells were processed through a machine (which resembles a dialysis machine) that removes mononuclear cells, a population of white blood cells that contains the CD-34s. He further processed the cells to select only CD-34s.
“These cells are very powerful repair cells for ischemic tissue. They are capable of forming new blood vessels,” Dr. Losordo said.
Then Dr. Losordo injected the CD-34 cells into the heart muscle. He first targeted where to inject the stem cells through a sophisticated electromechanical mapping technology that was originally developed by the Israeli army as a missile-tracking device. It identifies where the heart muscle is alive but not functioning because it is not receiving enough blood supply. This state is called hibernating myocardium. Via the mapping technique, the hibernating muscle appears as red, while the healthy muscle is blue.
“It’s the same way that bears hibernate because they want to decrease energy consumption,” Dr. Losordo said. “Muscle hibernates because it wants to decrease energy consumption to stay alive. So, it doesn’t contract. It’s not getting enough oxygenated blood to perform normally, so it shuts down its contractile function.”
Dr. Losordo has already launched a larger, national 20-center study that will enroll 150 participants to evaluate the promising therapy. He is also about to begin a similar study in heart failure patients using the same approach.
The study was supported by grants from the National Institutes of Health and Baxter Healthcare Corporation. Dr. Losordo is a consultant to Baxter.