Traffic Jam in Brain Causes Schizophrenia Symptoms: Researchers Reveal How Schizophrenia Works in the Brain and Provide a Fresh Opportunity for Treatment
 |
|
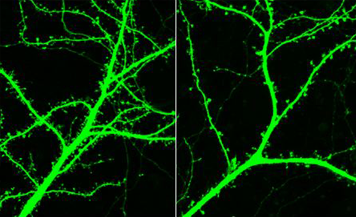
There are fewer pathways (green strands on right) for information to flow between neurons in the brain of a mouse bred to have symptoms of schizophrenia compared to a normal mouse. Fewer pathways cause the symptoms of schizophrenia. (Image by Peter Penzes) |
August 25, 2009 â Schizophrenia waits silently until a seemingly normal child becomes a teenager or young adult. Then it swoops down and derails a young life.
Scientists have not understood what causes the severe mental disorder, which affects up to 1 percent of the population and results in hallucinations, memory loss and social withdrawal.
But new research from the Northwestern University Feinberg School of Medicine has revealed how schizophrenia works in the brain and provided a fresh opportunity for treatment. In a new, genetically engineered mouse model, scientists have discovered the disease symptoms are triggered by a low level of a brain protein necessary for neurons to talk to one another.
A Traffic Jam in Brain
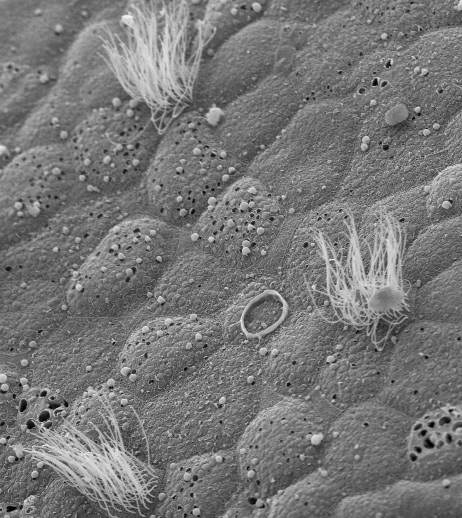
In human and mouse brains, kalirin is the brain protein needed to build the dense network of highways, called dendritic spines, which allow information to flow from one neuron to another. Northwestern scientists have found that without adequate kalirin, the frontal cortex of the brain of a person with schizophrenia only has a few narrow roads. The information from neurons gets jammed up like rush hour traffic on an interstate highway squeezed to a single lane.
“Without enough pathways, the information takes much longer to travel between neurons and much of it will never arrive,” said Dr. Peter Penzes, assistant professor of physiology at the Feinberg School. He is senior author of a paper reporting the findings published in a recent issue of the Proceedings of the National Academy of Science. Michael Cahill, a Feinberg doctoral student in neuroscience, is the lead author.
First Mouse Model to Develop Disease as a Teenager
Penzes discovered the kalirin effect after he created the mouse model, which was the first to have a low level of kalirin and the first to develop symptoms of schizophrenia as an adolescent (two months old in mouse time). This mimics the delayed onset of the disease in humans. In normal development, the brain ramps up the production of kalirin as it begins to mature in adolescence.
New Direction for Treatment
“This discovery opens a new direction for treating the devastating cognitive symptoms of schizophrenia,” Penzes said. “There is currently no treatment for that. It suggests that if you can stimulate and amplify the activity of the protein kalirin that remains in the brain, perhaps we can help the symptoms.”
Currently the only drug treatment for schizophrenia is an antipsychotic. “The drugs address the hallucinations and calm down the patient, but they don’t improve their working memory (the ability of the brain to temporarily store and manage information required for complex mental tasks such as learning and reasoning) or their ability to think or their social behavior,” Penzes said. “So you end up with patients who still can’t integrate into society. Many attempt suicide.”
Similarities Between Human and Mouse Brains
A few years ago in postmortem examinations of schizophrenic human brains, other scientists had found fewer connections between the brain cells in the frontal cortex and lower levels of kalirin. But the scientists couldn’t show whether one condition led to the other.
With the new mouse model, Penzes was able to demonstrate that the low level of kalirin resulted in fewer dendritic spines in the frontal cortex of the brain, the part of the brain responsible for problem solving, planning and reasoning. Other areas of the brain had a normal number of the dendritic spines. Human brains and mouse brains share many similarities in the way they function, Penzes said.
The new schizophrenic mouse model also exhibits more schizophrenic symptoms than other models, making these mice especially good for drug testing and development, Penzes said. The mice with low amounts of kalirin had a poor working memory, were antisocial and hyperactive.
Penzes said future studies would aim at enhancing the function of kalirin in the brain in an effort to correct the cognitive symptoms of schizophrenia.
To read the full study, visit Proceedings of the National Academy of Science: http://www.pnas.org/content/106/31/13058.full?sid=bde5ec32-a6b9-4735-bdfb-5b146d32cdac.
To learn more about Penzes’ research, visit: http://www.feinberg.northwestern.edu/penzes/.