July 8, 2003
Immune System Genes Stave Off HIV Infection
CHICAGO— Researchers have new answers as to why some HIV-infected individuals don’t progress to full-blown AIDS as rapidly as other HIV-positive people.
Northwestern University’s Feinberg School of Medicine scientist Steven M. Wolinsky, MD, and colleagues found that individuals with certain rare variations, or alleles, of two immune system genes—human leukocyte antigens A and B (HLA-A and HLA-B)—are better equipped to stave off HIV than people with more common sets of HLA alleles.
This finding indicates that HIV has evolved to attack the most common immune system genes and that there may be differences in how people respond to infection based on their HLA proteins. Importantly, the research, which was published in the July issue of Nature Medicine, showed that HIV influences human immune response just as humans put evolutionary pressure on the virus.
“We’re pushing on the microbe, and it’s pushing back on us,” Dr. Wolinsky said.
The group’s study, which involved 996 HIV-infected men in the Chicago component of the Multicenter AIDS Cohort Study (MACS), also has major therapeutic implications for determining the patients who require more aggressive treatment and for developing AIDS vaccines, Dr. Wolinsky said.
Dr. Wolinsky is the Samuel J. Sackett Professor and chief of infectious diseases at the Feinberg School and Northwestern Memorial Hospital. He also is director of the Great Lakes Regional Center for AIDS Research.
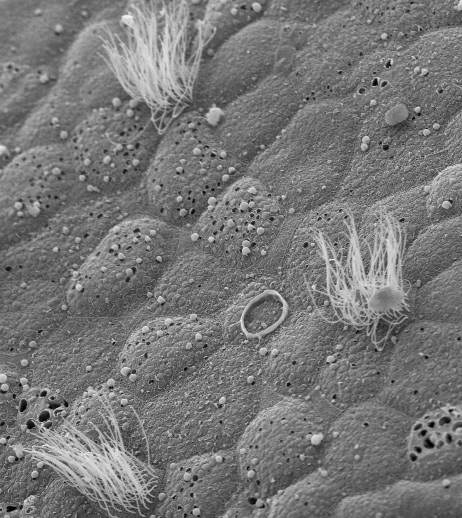
HLA molecules help trigger activity of infection-fighting T cells. During the immune response, HLA proteins bind bits of an invading microbe’s proteins in an infected cell, which are then presented on the infected cell’s surface to killer T cells. The killer T cells, also known as cytotoxic T cells, destroy the infected cell and thereby prevent spread of infection.
Importantly, the study demonstrated the first clinical application of a new statistical method, called minimum description length (MDL), that enabled the researchers to analyze the hundreds of HLA-A and HLA-B alleles found in the Chicago HIV study population and classify patients into disease progression groups based on their ability to bind specific microbial proteins. The investigators were then able to associate nine different HLA “supertypes” with disease outcome.
They found that men with the most frequent HLA supertypes had the highest viral loads—more HIV in their blood—while the men with the least frequent supertypes had the lowest. One of study’s more significant findings was that black men had lower viral loads than white men.
Findings from the study are especially pertinent to the development of AIDS vaccines. Since it appears that HIV has evolved to assail the most frequent alleles in the population, any vaccine designed to help killer T cells control HIV infection—which is based on the HLA—might not provide protection, Dr. Wolinsky said.
Further, because immune system alleles—and, thus disease progression rates—vary with different populations and geographical areas, it is therefore possible that AIDS vaccines will have to be tailored to specific locations or even for individual patients.
Wolinsky’s co-researchers were Elizabeth Trachtenberg, Children’s Hospital Oakland Research Institute; Bette Korber, Los Alamos National Laboratory; and Thomas Kepler, Duke University, among others.